Periapical lesions: Does the size of an endodontic lesion play a role in success and failure?
In modern dental practice tooth preservation still remains the treatment of choice when applicable. Dental implants have undoubtedly been a game changer for the modern clinician. Ethical guidance should always include a discussion of the treatment modalities available to the patient to alleviate the disease process.
There are many risk factors that dictate success and failure in endodontics. The single most important factor of success and failure can be predicated on the presence or absence of a periapical lesion at the time of treatment.1 Simply put, nonsurgical endodontic treatment of teeth without disease has a very high success rate that parallels dental implants.2
The success rate changes, however, when a periapical lesion is observed on a film. While teeth showing disease are still very treatable with root canal therapy, there is a marked decrease in the success rate by about 10%.3 This is likely due to a variety of factors beyond the scope of this article. Risk factors specific to each case also play a role in delayed healing or posttreatment disease. Despite all of these challenges, an apical periodontitis without periodontal communication can be thought of as an intrabony lesion. In terms of periodontal healing, these have the best success rates.4
Discussion
One risk factor that should be considered is the size of the apical lesion. Studies have shown that as lesion size increases, so does the risk for posttreatment failure of root canal therapy. This is likely because as the size increases, so does the likelihood that the lesion may have evolved to be cystic in nature.5 However, it should be noted that this is just a risk factor.
While it is impossible to tell if a lesion is cystic or granulomatous from a periapical radiograph or even a cone beam study,6 certain radiographic clues can help practitioners make the distinction.6 There also may be certain clues during treatment that could lead one to conclude that a cyst is being encountered or a granulomatous lesion merely exists.
Radiographically, a cyst will show a well-corticated border. During treatment, a straw-colored exudate may emanate from the canal, indicating the presence of cholesterol-containing clefts in the cystic fluid.7 Cysts and granulomas appear with approximately equal frequency, yet there does not seem to be a difference in the rate of healing and the findings may be inconsequential to treatment outcome.7
Case 1
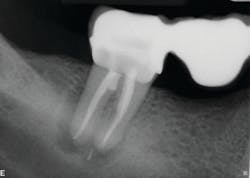
The first case involves a 49-year-old female. Tooth no. 31 had a deep periodontal probing on the straight buccal. The patient was warned that the tooth might be fractured, but she still decided on treatment (figure 1).
Calcium hydroxide paste medication was placed in the canals on three visits, each two weeks apart. Treatment included a total of six weeks of calcium hydroxide therapy.
The six-month recall showed nearly complete bone and furcation healing (figure 2). There is still some attachment loss on the straight buccal, but no. 31 remains asymptomatic and in good service.
Case 2
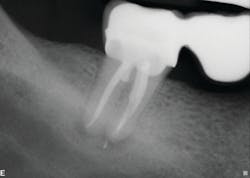
The second case involves a patient with tooth no. 19 having substantial furcation damage and moderate-sized apical periodontitis (figure 3).
Treatment included a two-visit approach, with two weeks in interim calcium hydroxide therapy.
Healing is noted on the six-month follow-up (figure 4).
Conclusion
Periapical lesion size can be thought of as a risk factor but not an absolute contraindication for endodontic therapy. It should be explained to the patient before treatment that the scope of therapy may include the combination of a surgical approach along with nonsurgical root canal therapy. However, many cases with large lesions end up healing quite nicely on their own without further intervention.7
References
1. Ng Y, Mann V, Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44(7):583-609. doi:10.1111/j.1365-2591.2011.01872.x.
2. Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30(12):846-850.
3. Swartz DB, Skidmore AE, Griffin JA Jr. Twenty years of endodontic success and failure. J Endod. 1983;9(5):198-202. doi:10.1016/S0099-2399(83)80092-2.
4. Kim CS, Choi SH, Chai JK, et al. Periodontal repair in surgically created intrabony defects in dogs: influence of the number of bone walls on healing response. J Periodontol. 2004;75(2):229-235. doi:10.1902/jop.2004.75.2.229.
5. Natkin E, Oswald RJ, Carnes LI. The relationship of lesion size to diagnosis, incidence, and treatment of periapical cysts and granulomas. Oral Surg Oral Med Oral Pathol. 1984;57(1):82-94. doi:10.1016/0030-4220(84)90267-6.
6. Rosenberg PA, Frisbie J, Lee J, et al. Evaluation of pathologists (histopathology) and radiologists (cone beam computed tomography) differentiating radicular cysts from granulomas. J Endod. 2010;36(3):423-428. doi:10.1016/j.joen.2009.11.005.
7. Lalonde ER, Luebke RG. The frequency and distribution of periapical cysts and granulomas. An evaluation of 800 specimens. Oral Surg Oral Med Oral Pathol. 1968;25(6):861-868. doi:10.1016/0030-4220(68)90163-1.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a newsletter for dentists and hygienists that focuses on periodontal- and implant-related issues. Perio-Implant Advisory is part of the Dental Economics and DentistryIQ network. To read more articles, visit perioimplantadvisory.com, or to subscribe, visit dentistryiq.com/subscribe.
About the Author

Doreen Toskos, DMD
Doreen Toskos, DMD, received her DMD degree from Harvard University in Boston, Massachusetts, following her undergraduate studies at Cornell University. She completed a two-year postgraduate residency in endodontics at Columbia University and has practiced on Long Island. She has lectured for general dentists and the New York Dental Association and is actively involved in continuing education. Dr. Toskos is an attending endodontist for the general practice and pediatric residency programs at Brookdale Hospital.

Joseph F. DiBernardo, DDS
Joseph F. DiBernardo, DDS, obtained both his undergraduate and dental degrees from Stony Brook University. He completed a general practice residency program at Nassau University Medical Center, and then a two-year residency program to specialize in endodontics at New York University in Manhattan. He worked as a general dentist for three years on Long Island and New Jersey. He then returned to Long Island to establish Smithtown Endodontics. Dr. DiBernardo is on staff at the general practice residency program at Stony Brook University Dental School.