Enamel microabrasion: A 40-year retrospective
What you'll learn in this article
-
How enamel microabrasion removes superficial intrinsic stains—such as fluorosis and idiopathic discoloration—through a controlled combination of hydrochloric acid and abrasives
-
Why enamel microabrasion is a minimally invasive, anesthesia-free treatment option that preserves tooth structure and eliminates the need for composite restorations in many cases
-
When to consider combining microabrasion with carbamide peroxide bleaching to enhance esthetic results for deeper or persistent enamel defects
-
How dental hygienists and general dentists can work together to identify candidates for microabrasion and educate patients on conservative treatment alternatives for white spot lesions
In 1984, Dr. Robert McCloskey reported about Dr. Walter Kane’s hydrochloric acid method of eliminating brown enamel fluorosis discoloration in Colorado patients in the 1920s.1 McCloskey rubbed HCl into the stained teeth of a patient, added a slight amount of heat, and eliminated most of their “Colorado Brown Stain.” The anterior teeth of one 16-year-old, named Evelyn, were treated by Dr. Kane in 1926. Her posterior teeth were not treated.
Sixty years later, in 1986, Dr. Theodore P. Croll visited 76-year-old Evelyn at her Colorado Springs home. A lateral aspect photograph documented the color-corrected anterior teeth juxtaposed with her brown, stained, untreated premolars and molars.2 Inspired by McCloskey’s report, Croll and Cavanaugh combined hydrochloric acid with laboratory pumice to create a mixture that would simultaneously erode and abrade superficial intrinsic enamel coloration and texture defects from human teeth.3,4 The term “dysmineralization” was coined for such intrinsic defects as fluorosis and idiopathic discoloration. Texture defects also could be improved. Experimentation with various acids in varying concentrations along with a variety of abrasives in a silica gel followed. Premier Dental Products Company produced PREMA Compound, and it was on the market for many years. Subsequently, Ultradent Dental Products introduced Opalustre Enamel Microabrasion Slurry. An insurance code was created for “Enamel Microabrasion – D9970.”
Additional reading: Incidence and prevention of white spot lesions during removable orthodontic treatment: A systematic literature review
A textbook5 and clinical and laboratory studies followed, and over the years, enamel microabrasion took its place as a routine consideration for treatment of teeth with superficial enamel discoloration.6-11
Dr. Renato Herman Sundfeld took a serious research and clinical interest in enamel microabrasion and introduced the method to patients and the dental literature in Brazil.
Combining enamel microabrasion with carbamide peroxide bleaching has been of key interest to Dr. R. Sundfeld and Dr. Daniel Sundfeld, and both have published extensively on this subject.12-14
This brief report documents the step-by-step method of accomplishing enamel microabrasion for a patient in her early 30s, who, in 2016, had a maxillary central incisor with a large white discoloration defect (figure 1).
The white defect had bothered her for years, but she declined to have the white spot cut away and the tooth restored with a bonded resin-based composite. Her children were patients in the office of the senior author (Dr. Croll), where she discovered, by photographs, the enamel microabrasion method. She was told that the white defect might penetrate too deeply for enamel microabrasion to succeed, but if it turned out not to be too deep, enamel microabrasion could be successful. The patient readily agreed to enamel microabrasion treatment. She was photographed nine years after treatment.
Another patient, who, as a 10-year-old, was pictured in the senior author’s textbook, had similar white dysmineralization of both maxillary central incisors. Enamel microabrasion color correction was accomplished and photographed five years later. Many years later, as an adult, the patient completed custom tray carbamide peroxide home tooth bleaching.
Technique
The patient consented to having the treatment photographed step by step. No local anesthetic injections were needed. Enamel microabrasion is pain free, and because an unrecognizable and minimal enamel surface is reduced, there is no sensitivity postoperatively. After placement of a rubber dam to isolate the incisor to be treated, a small bit of Opalustre compound was applied with gentle pressure using Ultradent’s Opal Cup (figure 2). The patient’s eyes were protected with eyeglasses (figure 3). Every 15 seconds or so, the compound was rinsed away, and the defect was evaluated (figure 4).
Upon removal of the white defect, topical fluoride solution was rubbed into the tooth surface with a cotton swab (figure 5). When the tooth surface was dry, a bit of residual white dysmineralization could be detected (figure 6). However, when the tooth surface was moistened with saliva (figure 7), the white enamel stain became virtually imperceptible from conversation distance (figure 8).
Nine years after treatment, there was no evidence that the white defect had been there (figure 9). The patient was advised that the white “flecks” on the labial surfaces of the other incisors and canine teeth could also be treated, but she declined, saying she “had not noticed them.”
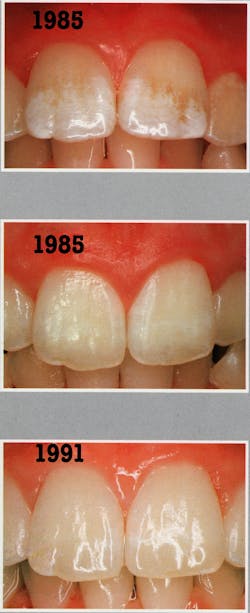
In 1985, a 10-year-old girl had white discoloration defects of both maxillary central incisors (figure 10–top). Note that Figure 10 images are taken from the senior author’s text, page 96.5 Using PREMA Compound, those mineral stains were eliminated (figure 10–middle), and the patient was photographed again five years later (figure 10–bottom). As an adult, the patient bleached her teeth with carbamide peroxide, 27 years after enamel microabrasion. In 2025, at a routine dentistry recall appointment for her four sons, she was again photographed, 40 years after enamel microabrasion and tooth bleaching (figure 11).
Aurelio de Oliveira Rocha et al. completed a “bibliometric review” of enamel microabrasion for treatment of white spot lesions. Their important review discovered that most reports were to evaluate clinical performance of enamel microabrasion, with Opalustre as the main product; fluorosis was the chief cause of the discoloration, most articles came from Brazil, and the chief authors of these works were R.H. Sundfeld and D. Sundfeld.15
Also by the author: Biomimetic/bioactive direct placement tooth restoration of premolars having preeruptive subenamel caries
Editor's note: This article appeared in the September 2025 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- McCloskey RJ. A technique for removal of fluorosis stains. J Am Dent Assoc. 1984;109(1):63-64. doi:10.14219/jada.archive.1984.0297
- Croll TP. A case of enamel color modification: 60-year results. Quintessence Int. 1987;18(7):493-495.
- Croll TP, Cavanaugh RR. Enamel color modification by controlled hydrochloric acid-pumice abrasion. I. Technique and examples. Quintessence Int. 1986;17(2):81-87.
- Croll TP, Cavanaugh RR. Hydrochloric acid-pumice enamel surface abrasion for color modification: results after six months. Quintessence Int. 1986;17(6):335-341.
- Croll TP. Enamel Microabrasion. Quintessence Publishing Co.; 1991.
- Berg JH, Donly KJ. The enamel surface and enamel microabrasion. In: Croll TP. Enamel Microabrasion. Quintessence Publishing Co.; 1991:55-60.
- Croll TP. Enamel microabrasion for removal of superficial discoloration. J Esthet Dent. 1989;1(1):14-20. doi:10.1111/j.1708-8240.1989.tb01032.x
- Croll TP. Enamel microabrasion for removal of superficial dysmineralization and decalcification defects. J Am Dent Assoc. 1990;120(4):411-415. doi:10.14219/jada.archive.1990.0127
- Killian CM, Croll TP. Enamel microabrasion to improve enamel surface texture. J Esthet Dent. 1990;2(5):125-128. doi:10.1111/j.1708-8240.1990.tb00627.x
- Donly KJ, O’Neill M, Croll TP. Enamel microabrasion: a microscopic evaluation of the “abrosion effect.” Quintessence Int. 1992;23(3):175-179.
- Killian CM. Conservative color improvement for teeth with fluorosis-type stain. J Am Dent Assoc. 1993;124(5):72-74. doi:10.14219/jada.archive.1993.0111
- Sundfeld RH, Croll TP, Briso AL, de Alexandre RS, Sundfeld Neto D. Considerations about enamel microabrasion after 18 years. Am J Dent. 2007;20(2):67-72.
- Sundfeld RH, Rahal V, Croll TP, De Aalexandre RS, Briso ALF. Enamel microabrasion followed by dental bleaching for patients after orthodontic treatment–case reports. J Esthet Restor Dent. 2007;19(2):71-77;discussion 78. doi:10.1111/j.1708-8240.2007.00069.x
- Sundfeld D, Pavani CC, Pini NIP, et al. Esthetic recovery of teeth presenting fluorotic enamel stains using enamel microabrasion and home-monitored dental bleaching. J Conserv Dent. 2019;22(4):401-405. doi:10.4103/JCD.JCD_77_19
- Rocha A, Cardoso K, Goebel MC, et al. A global overview of enamel microabrasion for white spot lesions: a bibliometric review. Restor Dent Endod. 2024;49(3):e29. doi:10.5395/rde.2024.49.e29
About the Author

Theodore P. Croll, DDS
Theodore P. Croll, DDS, is a diplomate of the American Board of Pediatric Dentistry. He is a 1973 Temple University School of Dentistry graduate. After serving in the US Army Dental Corps in Germany, he completed pediatric dentistry training at the University of Connecticut in 1978. Dr. Croll’s Doylestown, Pennsylvania, pediatric dentistry practice merged with Doc Bresler’s Cavity Busters in December 2018. He currently is clinical professor of pediatric dentistry at Case Western School of Dental Medicine.
Renato Herman Sundfeld, DDS, PhD, MS
Renato Herman Sundfeld, DDS, PhD, MS, is a 1980 graduate of Araçatuba Dental School, UNESP and a professor of restorative dentistry at Araçatuba Dental School, UNESP – Univ Estadual Paulista, Araçatuba, SP, Brazil. Along with teaching, he has extensive clinical experience in research regarding resin bonded sealants, along with enamel microabrasion.
Daniel Sundfeld, DDS, PhD, MSc
Daniel Sundfeld, DDS, PhD, MSc, is a 2010 graduate of Piracicaba Dental School, UNICAMP and a professor of restorative dentistry at Maringá Dental School, UEM – Univ Estadual de Maringá, Maringá, PR, Brazil. Dr. Sundfeld has followed in his father’s footsteps teaching students of dentistry and researching topics in clinical dentistry, including enamel microabrasion.