Taking the mystery out of cementation decision making
Marshall D. Fagin, DDS
How can we simplify the decision-making process for cementation selection and better understand the advantages of each type of cement that's available? Is there a risk in using one cement for everything? In this article, I'll review some of the current resin cements on the market.
There are three key considerations to start with:
1. The type of restoration; e.g., crown, onlay, veneer, etc.
2. The material being used; e.g., lithium disilicate, zirconia, metal, etc.
3. The tooth preparation design
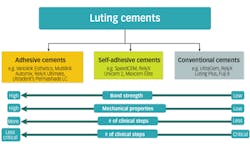
With that in mind, let's look at three categories: resin-modified glass ionomer (RMGI), self-adhesive, and adhesive cements (figure 1).1
MORE READING |Cements for pediatric dentistry: What are clinicians using and why?
Resin-modified glass ionomer cements
Like conventional cements, RMGI cements are dependent upon mechanical retention, so they require preparations taller than 4 mm and a taper of 8 degrees or fewer.2 They are more moisture tolerant than the other resin cements, so I recommend them when good isolation is not possible. The RMGI cements such as UltraCem, FujiCEM, and RelyX Luting Plus provide fluoride release, which is helpful for patients with a higher caries index.1,3 These cements are recommended for luting most indirect restorations except veneers. They are not indicated for feldspathic and leucite ceramics, which last longer with adhesive cements.2
Self-adhesive cements
Self-adhesive resin cements eliminate the need for separate conditioning with phosphoric acid and bonding agents. Ivoclar's SpeedCEM, Kerr's Maxcem Elite, GC America's G-CEM, and 3M-ESPE's RelyX Unicem are examples that offer this simpler protocol. Although these cements provide chemical bonding and improved bond strength compared to conventional luting cements, their properties are inferior to adhesive cements.2,4,5 Higher-strength ceramics, such as lithium disilicate and zirconia, can withstand loads without adhesive cements, but one then loses other advantages of these cements.
MORE READING |Making cementation simple and predictable with self-adhesive resin cements
Adhesive cements
Adhesive resin cements require separate bonding steps, but they offer the benefit of enhanced bond strength.2,4,5 This is critical for preparations with nonretentive forms, such as veneers or short clinical crowns. They may be further categorized as light cure, dual cure, and self cure. Light-cured resin cements (e.g., Ivoclar's Variolink Esthetic LC, Ultradent's PermaShade LC, and 3M-ESPE's RelyX Veneer) are indicated for thin, highly translucent anterior restorations. These cements are often color stable and provide a long working time. Self-cure resin cements (e.g., Panavia F2.0) do not require light for polymerization and are indicated with opaque restorations, such as thick full-contoured zirconia, metal, PFM, and endodontic posts. Dual-cure resin cements (e.g., Ultradent's PermaFlo DC, Variolink Esthetic DC, Multilink Automix, and RelyX Ultimate) can be light cured and self cured; however, light cure is recommended so as to achieve the best bond. Regardless of the type of cure, adhesive cements are aided by etching and bonding of the tooth surfaces.1
Figure 1: Cement categories with some of the advantages and disadvantages of each
Try-in pastes
Where esthetic outcomes are important, cement selection with shade options can impact the esthetic result (figure 2). Try-in pastes prove helpful, especially where there are differences in ceramic thickness or stump shades are different between adjacent teeth. After using try-in pastes with a few cases, you will discover how little additional time is needed to accomplish greatly improved results.
Figure 2: Demonstration of shade difference between try-in pastes on typodont with Variolink Esthetic Warm+ and Light+
Pretreatment of the restorations
Zirconia can be made a better candidate for bonding when treated with airborne particle abrasion and tribochemical silica coating (Danville's SilJet).6 Lithium disilicate is best pretreated with hydrofluoric acid. Unfortunately, these pretreatment regimens are compromised by saliva after trying them intraorally. Prior to final cementation, I recommend decontaminating the restoration using a product such as Ivoclar's Ivoclean (figure 3). A silanating agent (e.g., Monobond Plus from Ivoclar Vivadent)2 is then placed inside the ceramic restoration (figure 4).
Figure 3: To decontaminate the restoration, rinse, then scrub with Ivoclean, leave for 20 seconds, and rinse.
Figure 4: Place silanating agent, allow to react for 60 seconds, and then disperse excess by air drying.
Preparing the tooth for bonding
Etch-and-rinse techniques with phosphoric acid create the strongest bond strength, but it comes with the higher risk of postop sensitivity. A universal bonding agent (e.g., Ivoclar's Adhese Universal) offers etch and bond in a single step, thereby reducing sensitivity. With all options, use a desensitizing agent with glutaraldehyde, such as MicroPrime G (Danville Materials) or Gluma (Heraeus Kulzer). It is recommended that you apply two one-minute applications (suction off after each; do not rinse).7,8 An excellent resource summary of these techniques is presented by Gordon J. Christensen, DDS, MSD, PhD, in his Dental Economics article titled "Which technique is best-total-etch, self-etch, or selective-etch?"
So what cements do you need in your office?
Figures 5 and 6: Tack-cure Variolink Esthetic cement for two seconds per quarter for ease of cement cleanup. After cleanup, place liquid strip (glycerin gel) to protect the oxygen inhibitor layer. Then final cure all of the crown for 10 seconds, followed by final cleanup; adjust and polish.
Adhesive resin cement is a must to have available for all ceramic restorations, veneers, inlays, and onlays. Having this in light-cure and dual-cure materials provides flexibility of technique (figures 5 and 6). Having an RMGI cement offers a simplified technique along with fluoride protection, and having a conventional cement where enhanced retention and bond strength are not needed provides a second choice.3,8 For metal crowns, dual-cure and self-curing cements are also options. However, one may want to avoid the challenge of future crown removal such as when adhesive resin cement is combined with cutting off ceramic crowns, thus considering conventional cements where retention is not an issue and color modification is not needed.
Another desirable property of a cement is its radiopacity. This is especially important with implant restorations. Do your research and know the comparative level of radiopacity. Radiographs taken at the time of delivery, after cement cleanup, will show areas of excess cement that are missed. However, it is highly recommended to design custom abutments with margins at or above the crest of tissue for ease of thorough cleanup.
Even when we do all the right things, failures still sometimes occur. It's always about how to maximize success and work efficiently and with the least pulpal trauma. Try to meet minimum thickness requirements of restorative material for strength and have rounded line-angles with all ceramics. Most important is to remember to read all instructions carefully and follow them well. And to keep it simple, once you have your two to three cements selected for your office, create a list of what you would use each one for and why. Then, you can move forward quickly and with confidence.
References
2. Singhal S. Cementation navigation. Dental Lab Products. 2012;37(7):18-19.
3. Dehghan M, Braxton AD, Simon JF. An overview of permanent cements. Inside Dentistry website. https://www.dentalaegis.com/id/2012/11/an-overview-of-permanent-cements. Published November 2012.
4. Shillingburg HT, Whitsett LD, Jacobi R, Brackett SE. Cements. In: Fundamentals of fixed prosthodontics. 3rd ed. Chicago, IL: Quintessence; 1997:400-405.
5. Shull F, Singhal S. Cementation simplified: Reliable protocols for cementing and bonding today's restoration [continuing education course]. Dentaltown website. http://www.dentaltown.com/Dentaltown/OnlineCE.aspx?action=DETAILS&cid=306. Published 2012.
6. Tzanakakis EG, Tzoutzas IG, Koidis PT. Is there a potential for durable adhesion to zirconia restorations? A systematic review. J Prosthet Dent. 2016;115(1):9-19.
Marshall D. Fagin, DDS, is a practicing prosthodontist in Buffalo, New York. He is also a part-time associate professor at the State University of New York at Buffalo Dental School Postgraduate Prosthodontics and lectures internationally. Contact him at [email protected].