Challenges to be solved in clinical dentistry
Key Takeaways
-
Digital Radiography Needs Better Resolution
Current digital radiographic sensors fall short of analog film in detecting early caries and fine anatomical details, impacting diagnostic accuracy and treatment planning. -
Cariostatic Restorative Materials Are in Demand
Composite resin dominates clinical use but lacks longevity. There's an urgent need for a strong, esthetic, tooth-colored material with fluoride release and better handling properties. -
Rethink Resin Cements for Crowns
Resin cements shrink and open margins to plaque and debris. Clinicians should favor RMGI or glass ionomer cements for their cariostatic benefits and lower sensitivity risk. -
3D Printing and Scanner Tech Need Upgrades
In-office 3D printers and intraoral scanners require better accuracy, smaller sizes, infection control improvements, and more durable resins for long-term use in restorations. -
Endodontic Sealers and Implant Materials Still Lag
Current sealers don’t reliably seal dentinal tubules, contributing to root canal failures. Also, zirconia implants may reduce peri-implantitis compared to titanium, but more comparative research is needed.
Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
Q: I am a general practitioner with 25 years of practice experience. I still see numerous clinical areas that have challenges and need improvement. Why are so many of the research projects I see on unimportant subjects unrelated to clinical diagnosis, caries and periodontal disease prevention, occlusion, and very importantly, treatment? What do you feel still needs improvement in clinical dentistry, and what could possibly be done to improve those categories?
A: Some of the significant challenges to relevant research are difficult to solve because of significant government regulations, lack of adequate funding, and lack of experienced research and development staff. As you may know, Clinicians Report Foundation has been evaluating products and informing the profession about their findings for nearly 50 years. Each year, we spend considerable time determining what topics in dentistry need further research and what new methods could improve patient care.
The following information includes some items we have identified that could and should be improved.
Accuracy of digital radiographic sensors
Experienced dentists, including myself, often compare current digital radiographic images with analog film images of the past. It is easily apparent to the naked eye that analog film shows more detail and accuracy. This deficiency can be problematic relative to identifying initial caries and many other features. Enhancing the digital images helps interpretation of anatomy and restorations but does not satisfy the challenge. Typical general dentists and hygienists make many radiographic images per day. Misinterpretation of images and lack of proper treatment plans and treatment are often the result (figures 1–3).
Cariostatic restorative materials
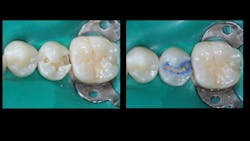
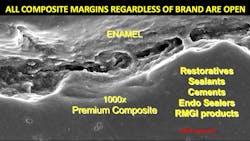
Composite resin is the most-used restorative material. Most general dentists place many composites every clinical day. Tooth restorations made with composite resin are well known to have shorter longevity than the now little-used amalgam (figures 4–7).
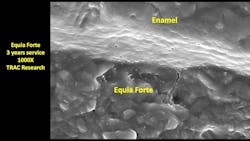
Recent advancements in glass ionomer and resin-modified glass ionomer (RMGI) have helped significantly, but these materials need to have higher strength, less solubility and wear, greater longevity, and easier working characteristics. Dentistry is in dire need of an esthetic, cariostatic, easily placed and finished, tooth-colored restorative material.
Cariostatic cements
Today’s ceramic crowns have some good characteristics accompanied by some challenges. Most ceramic crown margins are more open than well-placed cast-gold alloy restorations. Current resin cements shrink significantly, adding more opening for ingress of food debris, plaque, and microorganisms (figure 8). RMGI cements have cariostatic properties, as do conventional glass ionomer cements. They should be used whenever possible instead of noncariostatic resin cement. Easily placed, cariostatic, nonsensitivity-producing, low-solubility, tooth-colored cement is needed immediately!
Remineralizing materials
Although some products claim remineralization, Clinicians Report Foundation in vivo studies have shown minimal to no remineralization, primarily because of lack of patient compliance. This concept needs additional basic research, development of new products, and in vivo real-world long-term research.
Improvements in scanners
Although scanners are gaining in popularity because of relative ease of use and patient preference over elastomers, they need significant improvements. A few example needs are lower cost, much smaller size, elimination of keyboards (which are inadequate relative to infection control), significantly better accuracy (especially cross-arch), and easier sterilization/disinfection. Although current scanners claim accuracy, that claim is not evident when compared to conventional analog impressions.
Endodontic sealers that seal
This concept has been studied by many, and apparently still needs more research and development. Human teeth have thousands of microscopic dentinal canals. Additionally, teeth are an open system from the pulp to the tooth external and the oral cavity.
Clinicians Report Foundation has shown that the seal provided by endodontic sealers is minimal to none. Is that why endodontic procedures that initially look good radiographically often fail? Endodontic procedures vary around the world. It would be desirable if the various techniques could be compared to one another and improvements made.
Implant material
Is titanium alloy the best implant material, or are zirconia implants serving better than metal? Peri-implantitis is now well-known and observed routinely on titanium alloy implants. Those using ceramic implants claim less peri-implantitis. Recently, those using small-diameter, one-piece implants are claiming less or no peri-
implantitis. Isn’t it about time that interested, knowledgeable researchers conduct animal studies to scientifically determine what material is best for dental implants?
Improvements in 3D printers
Currently, 3D printers are slowly growing in clinical office use. They are already widely used in dental laboratories. Although some companies are promoting 3D printing for dental crowns, labs report this concept is being used primarily for techniques needing only short-term use. The most common uses are study models, occlusal splints, surgical guides, temporary restorations, and similar short-term need items. Selective laser melting is now being used for making successful removable partial denture frameworks by most labs.
However, printing of crowns, fixed prostheses, and other long-term items have been slow to be incorporated by clinical offices, and resin crowns and fixed prostheses are in low demand by dentists. Stronger, more wear-
resistant, more esthetically acceptable resin materials are needed to make the printing concept more useful, trusted, and popular.
In my opinion, a strong, slightly wear-prone esthetic crown would be better than a zirconia crown as an implant-supported restoration. Such crowns placed on implants wear into proper occlusion, which is nearly impossible for zirconia crowns on implants.
Laser improvements for tooth cutting
I have been investigating laser use for several decades. Some laser wavelengths cut soft tissue and bone well. But with a few exceptions after trying lasers for tooth cutting, most practitioners return to burs because of the slow speed to make tooth preparations with a laser.
The ability for lasers to make tooth preparations without anesthesia is an attractive characteristic for a few laser types. Some dentists, especially pediatric dentists, accomplish most tooth preparations with a laser. The CO2 Solea laser is a desirable but expensive one that is capable of slow but nearly painless tooth cutting. Most dentists who have a laser have a diode laser, which does not cut with the laser beam but can cut soft tissue with heat.
A small, relatively inexpensive laser that can cut tooth structure is needed and would be a desirable instrument for most dentists.
Summary
Dental diagnostic and preventive procedures, restorative and surgical procedures, and research have advanced markedly in recent years. But many of the technologies, materials, and techniques have become stable without apparent efforts to increase their adequacy. This article includes a few of those topics, some of which need immediate attention and others that demand long-term research and new development.
Editor's note: This article appeared in the June 2025 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.