What is the best type of crown prep?
Key Highlights
- Crown preparations must now be material-specific, accounting for digital scanning, lab die spacing, occlusion, and esthetic demands to reduce debonding, caries, and fracture risk.
- Full-strength (3Y) zirconia dominates crown use and demonstrates exceptional long-term strength but requires slightly deeper axial and occlusal reduction due to virtual die spacing.
- Esthetic zirconia and lithium disilicate (e.max) demand deeper, more precise preparations than 3Y zirconia to compensate for lower strength and minimize long-term breakage.
Each month, Dr. Gordon Christensen answers a question from readers about everyday dentistry.
Q: The new generation of ceramic crowns is now dominant. I am finding clinical challenges such as crowns coming off, caries developing on the margins, and occasionally crowns breaking. Although I know there are numerous factors potentially causing these problems, I feel that most are related to tooth preparation for crowns. I would appreciate knowing your personal thoughts on the desirable characteristics for ideal crown preps.
A: You are certainly correct! It is my observation that a crown prep is no longer a crown prep. There are several necessary types of preps directly related to at least the following factors:
- Type of material used for the crown
- Tooth or implant
- Patient’s occlusion
- Esthetic needs
- Laboratory spacing of the die
- Cement
Providing details about the challenges of each issue would be a major project. Instead, I will relate the needed preparation characteristics for the materials currently being used for most crown restorations.
Using data from one of the largest dental laboratories in the world, Glidewell, the following types of crowns for 2024 are as follows (data from Darryl Withrow, Glidewell):
- Full cast 1.5%
- Ceramic over zirconia 2.0%
- Full-strength zirconia 65.8%
- Esthetic zirconia 18.9%
- e.max 6.1%
- Composite 0.2%
- PFM 5.4%
Currently, zirconia, either full-strength or esthetic zirconia (with more yttria in it), is the primary material used by Glidewell, which is active in many diverse geographic areas.
The use percentage of full-strength zirconia is relatively stable; esthetic zirconia use is increasing; e.max, ceramic placed over zirconia, and PFM are declining; and use of full-cast and composite are negligible.
I will focus on crown prep characteristics for full-strength zirconia, esthetic zirconia, and e.max (lithium disilicate).
Current challenges related to the following tooth preparation characteristics
Almost all impressions are now scanned, whether the dentist scans the mouth or the lab scans an elastomer impression. When scanning, a typical lab spaces the virtual prep about 60 microns on the axial walls and up to 500 microns (0.5 mm) on the occlusal table. This spacing subtracts from the potential thickness of the restorative material being used, requiring the dentist to make the prep slightly deeper on all axial walls and up to 0.5 mm deeper on the occlusal surface.
Full-strength zirconia, commonly known as 3Y zirconia
In vivo long-term research by Clinicians Report Foundation (CR) has shown this material to have remarkable lack of breakage over more than a decade in the mouth.
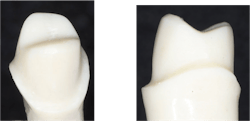
No 3Y posterior tooth crowns made by more than 20 labs and seated by various clinicians have broken over the approximately decade of service. CR research has shown that 3Y zirconia can be as thin as 0.3 mm and not have breakage in the mouth. Figure 1 shows tooth preparation characteristics before scanning impressions became the norm and other materials were also used. Figure 2 shows the reason for changes in tooth preparations caused by scanning and spacing that have evolved over a decade of use.
Tooth preparation characteristics for zirconia started out as:
- 2 mm occlusal reduction
- At least 1 mm reduction on all axial walls
- A moderate-depth margin chamfer about 0.5 mm
- Twenty degrees or less lack of parallel from the long axis of the tooth
However, because of spacing of virtual dies by labs, dentists must prepare teeth for 3Y zirconia slightly deeper on the axial walls (60 microns is slightly thicker than a typical human hair) and moderately deeper on the occlusal (up to 500 microns is about 10X more than the thickness of a human hair) (figure 2).
Esthetic zirconia and lithium disilicate (e.max)
In vivo long-term research by CR described previously has shown some breakage of both e.max and several brands of esthetic zirconia over more than a decade in the mouth (up to 7.0%). Details are available from CR on request.
This data should not discourage practitioners from using these more esthetic materials when esthetic concerns are present, but patients should be advised to use care when chewing hard foods. 3Y zirconia is advised for molars to avoid this challenge.
Figure 3 shows the tooth preparation characteristics needed for these material types that have evolved over a decade of using scanners and die spacing. They are:
- 2 mm or more occlusal reduction
- At least 1.5 mm reduction on all axial walls
- A moderate-depth margin chamfer about 1.0 mm
- Twenty degrees or less lack of parallel from the long axis of the tooth
Because these materials are somewhat weaker than 3Y full-strength zirconia and have some breakage in service, the tooth preparations should be deeper than for 3Y zirconia (figures 3 and 4).
Summary
As observed nationally in labs, improving tooth preparations could be the solution to reduce most of the observed maladies with the dominant zirconia and lithium disilicate crowns. Crown preparations have changed significantly since scanning impressions have become state of the art. They vary according to the materials selected for use in specific situations, the occlusion, esthetic needs, and obtaining normal tooth anatomy.
Editor's note: This article appeared in the February 2026 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.