Prevention of iatrogenic issues in anterior restorations
When dentists embark on cosmetic improvements for our patients, our goal is to improve the patient’s appearance, self-confidence, and dental health without causing additional problems. One of the hardest tasks we have as professionals is when a patient presents with a situation that was directly caused by previous dental treatment, whether our own or someone else’s. A delicate conversation follows: we should assure the patient we are there to help, but we should not comment on the past dental treatment if we do not know all of the facts. If we caused the issue, we should just correct it for the patient. If it was done elsewhere, we should keep the discussion to the facts and correcting the patient’s issues.
Case report
A 52-year-old female patient presented to my office with recent porcelain restorations that had been placed on her upper six anterior teeth. Besides her complaint of the bite feeling different, her main concern was that her speech was off, especially her s sounds. She stated these problems occurred after the final crowns were placed. Further questioning also revealed that she was unhappy with color and shape (figures 1–3). A full examination was completed, including x-rays and photographs, and periodontal, TMJ, occlusion, and dentition evaluations. She had excellent oral health and her dental issues were all related to her occlusal and esthetic complaints.
Figure 1: Anterior smile view of the patient’s original restoration
Figure 2: Anterior retracted view of the patient’s original restoration
My diagnosis was that the final anterior restorations induced an anterior constriction. Her mandible was forced posteriorly from overcontoured excess lingual porcelain on teeth Nos. 7–10. In addition, her tongue did not have enough room to move forward for proper speech enunciation, especially with her s sounds. The initial treatment involved placing the patient in a Kois Deprogrammer appliance. 1 This would allow her mandible to move in a position dependent on the muscles and remove the interferences caused by her dentition and the excess lingual porcelain. The patient returned one week after wearing the appliance and stated that she felt great, her jaws were comfortable, and she liked their position. Diagnostic models were taken in her centric relation position with the appliance in place and mounted on a Panadent articulator. A diagnostic equilibration was completed on the models. The final equilibration would be completed after an additional three weeks.
Figure 3: Maxillary occlusal view of the patient’s original restoration
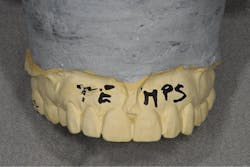
After the equilibration was completed and the lingual porcelain reduced on the anteriors, the patient felt “back to normal.” Diagnostic models of the refined occlusion were taken, along with measurements using the Kois Dento-Facial Analyzer facebow (Panadent), and sent to the lab for a diagnostic wax-up. The lab was instructed to keep the lingual surface the same to prevent the speech issues from returning. The lab technician was also given direction on incisal edge position and other esthetic corrections.2 The diagnostic wax-up was returned with a putty matrix and a vacuform stent (figure 4). The putty was used to try in the proposed treatment directly in the patient’s mouth with bis-GMA provisional resin. She gave approval on the proposed treatment and liked the esthetic improvements. The final color was chosen, and the patient was appointed to correct gingival levels on the central incisors with a hard-tissue laser crown-lengthening technique.
Figure 4: The diagnostic wax-up
The Waterlase MDX (Biolase) was used for the surgical osseous crown lengthening, along with necessary soft-tissue refinements.3 The patient was given post-op instructions and returned one week later so we could monitor healing. The gingival tissue was allowed to completely heal for 90 days. The patient returned around the 70-day mark and was examined and scheduled for the longer appointment of crown preparations. The patient decided that she would like to have a nicer smile and wished to have a much lighter color and to treat additional teeth. The upper 10 anterior teeth were going to be treated initially.
The patient returned for the preparation visit. The existing crowns were removed and the teeth, including the additional bicuspid teeth, reprepared. A final impression was taken with a PVS impression material, Imprint 4 VPS (3M Oral Care) heavy body and light body, and Impressiv (Cosmedent). The provisional crowns were fabricated from the putty matrix with bis-GMA resin (Mirror Image, Cosmedent) and seated with a temporary cement (figure 5). Additional models were taken of the temporary crowns and a facebow was taken of the provisionals (figure 6). A bite was taken against the opposing arch with both the prepared teeth and the temporaries. This was sent to the lab with instructions to fabricate the crowns with layered lithium disilicate. IPS e.max Press (Ivoclar Vivadent) was used.
Figure 5: The provisional crowns during try-in
Figure 6: A model of the temporary crown
The patient returned three weeks later for the final insertion. The temporaries were removed and the preps cleaned with air abrasion, using 27-micron aluminum oxide.4 Retraction cord impregnated with aluminum chloride was placed.
The options for proper cementation must be carefully considered ahead of time. The cementation can be cohesive or adhesive. The decision was made to use an adhesive cementation process. The cement that was used was Bisco’s eCement. Since the crowns were fabricated, this dual-cure cement ensured a complete cure. The formulation is available in a single-stage cure for veneers and a dual-stage for crowns, as well as several shades.
The enamel was selectively acid etched with Select HV Etch (Bisco). This is a 35% high-viscosity phosphoric acid etchant available with benzalkonium chloride, an antimicrobial agent that does not slump. The teeth were then treated with All-Bond Universal (Bisco), which is a light-cure bonding agent that is compatible with light, self and dual-cured cementation materials. The manufacturer’s instructions were followed.5 The eCement was then placed in the crowns and cured for 2 to 3 seconds only. The excess cement was removed, and the final cure was completed. The teeth were seated two at a time, starting with Nos. 8 and 9. After all crowns were seated, final cleanup was completed, occlusion was verified, and minor esthetic correction was completed (figures 7 and 8).
Figure 7: Anterior retracted view of the patient’s final restoration
Figure 8: Anterior smile view of the patient’s final restoration
Treatment of patients with ceramic restorations requires proper planning for both esthetics and function. After all other details are planned and completed, it is the final insertion process and the proper occlusal scheme that determine how long the ceramic material will survive in the mouth. Proper cementation material and technique are critical for patient comfort as they eliminate sensitivity and ensure long-term success. Dentists should find the cementation process and materials that work best for them and become familiar with the process. Successful long-lasting restorations allow for happier patients and reduced stress for everyone involved.
Author’s note: Dr. Peck discloses that that he was paid an honorarium for this article. He uses all materials discussed in daily practice.
References
1. Beshar MJ. Systematic treatment using a direct deprogrammer to resolve long-standing problems in a phobic patient. Compend Contin Educ Dent. 2015;36(6):418-425.
2. Malik K, Tabiat-Pour S. The use of a diagnostic wax set-up in aesthetic cases involving crown lengthening—a case report. Dent Update. 2010;37(5):303-307.
3. Chu SJ, Tan JH, Stappert CF, Tarnow DP. Gingival zenith positions and levels of the maxillary anterior dentition. J Esthet Restor Dent. 2009;21(2):113-120.
4. Chaiyabutr Y, Kois JC. The effects of tooth preparation cleansing protocols on the bond strength of self-adhesive resin luting cement to contaminated dentin. Oper Dent. 2008;33(5):556-563.
5. Passia N, Lehmann F, Freitag-Wolf S, Kern M. Tensile bond strength of different universal adhesive systems to lithium disilicate ceramic. J Am Dent Assoc. 2015;146(10):729-734. doi: 10.1016/j.adaj.2015.04.008.
Fred H. Peck, DDS, AAACD, is a third-generation dentist practicing in Cincinnati, Ohio. He is a fellow of the International College of Dentists, a Kois Center graduate, and a mentor for Cerecdoctors.com. He has published numerous articles and presented topics at several major dental meetings on cosmetic dentistry, dental lab communication, and direct resin bonding, including hands-on seminars.