Diagnostic challenges of dental radiographs and adjunctive methods of caries identification
Ask Dr. Christensen
Q+A
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics readers. If you would like to submit a question to Dr. Christensen, please send an e-mail to [email protected].
Q:
I am a mature practitioner, having practiced for 30 years. Early in my career, bitewing and periapical radiographs provided relatively good observation and identification of initial dental caries, and I did not miss many lesions. However, now I find that I often miss initial caries, and I am embarrassed on subsequent recall appointments to find significant, large lesions that I overlooked on earlier appointments. It seems to me that the current expensive digital sensors should offer better diagnostic capabilities than I am seeing. I am convinced that the analog radiographs that I used early in my career were much more diagnostic. What has happened to dental radiographs? What can I do to better identify initial caries?
A:
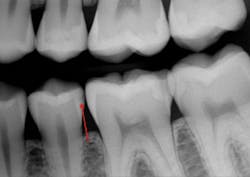
Your observations are shared by the majority of mature practitioners. Many younger practitioners have not noticed the inadequacy of periapical and bitewing radiographs because they do not have a historical perspective relative to the problem you described. I recently received a typical example from an excellent general practitioner in the eastern part of the US (figures 1 and 2).
Upon initial examination of the radiograph, only a few minor lesions were observed. When the dentist excavated the caries in the maxillary second molar, the extreme depth of the lesion was able to be seen. This is not an abnormal finding. In spite of the ability to manipulate digital images through magnification, coloring, texturing, and change of contrast, most small lesions and some large lesions are often missed.
In this column, I will discuss the problems caused by the inadequacy of dental radiographs and present some relatively effective ways to partially overcome these problems. It is my intent to continue to motivate manufacturers of digital sensors to improve the diagnostic capabilities of their products.
Figure 1: Note the lack of any clearly identifiable presence of deep carious lesions on this current-generation digital radiograph.
Figure 2: On making the initial opening of the mesial surface of the second maxillary molar, the extreme depth of the lesion is evident.
Clinical problems associated with inadequate digital radiographs
Pulpal death: Some patients are diligent with the consistency of their six-month dental checkups, while others are not. In an active-caries patient, when significant-depth lesions are missed, waiting longer than a normal six-month recall period can easily result in necessary endodontic treatment. If deep lesions are missed at a six-month checkup, even conscientious patients can require endodontic treatment that could otherwise have been prevented.
Large tooth preparations: It has been proven and is well-known among practitioners that large direct restorations of resin-based composite or amalgam have significantly shorter clinical longevity than small restorations. Inadequate radiographs certainly contribute to longer waits before restoring teeth, and ultimately lead to more premature failure of large restorations. Subsequent replacement of the failed restorations further weakens the tooth and can cause additional failure. This lack of adequate radiographs costs patients.
Necessity for crowns: In the US, the cost of an indirect restoration is about 20% of the fee for an extracoronal indirect restoration. Allowing caries to grow in size often necessitates placing crowns on the affected teeth. The result is higher costs for patients.
Additional clinical time for dentists: A small Class II resin-based composite can usually be placed in a short time, while larger composites require much more time and expertise (figure 3). Third-party payers pay the same regardless of the size of the restoration. If lesions are not identified early, the dentist must spend more time preparing the tooth and then placing and finishing the restoration. Not only does the patient suffer shorter restoration longevity, additional future replacement of the restoration, and higher cost, but the dentist also expends more time and effort for a large restoration and receives less proportionate revenue for the services (figures 4a and 4b).
Figure 3: Note the presence of a lesion on the distal surface of the mandibular second premolar, which appears to be about halfway through the enamel. Most current digital radiographs show only about half of the actual depth of initial caries as shown in the partly finished prep. The lesion was already into the dentin about 1 mm as shown on this partially completed tooth preparation.
Additional material cost for restorations: Restorative resins and accessory placement materials are expensive. Large restorations have more overhead costs for dentists because more resin is used, liners or bases are often needed, and more complex matrices are needed.
Cost of the challenges caused by inadequate radiographs: Typical general dentists place several direct restorations per day. The inability to diagnose initial caries on dental radiographs at the most opportune time for restoration is a reality dentists observe every clinical day. Both patients and dentists suffer the previously described circumstances because of this problem. Dentists, professional dental organizations, inventors, and manufacturers must exert the effort, time, and money to overcome this problem.
Figures 4a and 4b: The restored premolar tooth is the same premolar shown in Figure 3. Such small restorations serve far longer than large ones as shown in the molar.
What can be done before radiographs are improved?
There are numerous caries detection concepts and techniques available, with costs ranging from relatively low to high. However, it is my observation that few dentists have taken the time and spent the money to incorporate them into their practices. I will list onlythe relatively simple and inexpensive ways to detect caries. Keep in mind that there are many other devices and concepts available, but few have found significant acceptance by practitioners.
I suggest that you analyze the following products on the internet and at the next large dental meeting you attend to determine which best fits your mode of practice. The concepts listed here have been well accepted by most practitioners who have incorporated them into their practices.
Transillumination
Clinicians Report Foundation researchers have determined that the following two devices identify initial proximal caries better than the current generation of radiographs:
- Microlux 2 Transilluminator from AdDent Inc., is a simple, low-cost, battery-powered transilluminator. It shows initial proximal caries in nonrestored anterior and posterior teeth.
- DEXIS CariVu from Henry Schein uses near-infrared transilluminated light to show the extent of proximal caries. The cost is about the same as a digital sensor.
Adjunctive methods to identify caries
The Cavitron Prophy Jet Air Polishing System from Dentsply Sirona and similar devices are well-known, but they could be used more. I suggest these devices be used not only to remove stains and plaque on teeth, but also for Class I caries detection. The sodium bicarbonate slurry that is emitted cleans plaque and stains easily from occlusal surfaces, but it does not effectively get into cavitated Class I caries. The resulting pigmentation remains in the cavitated areas on the occlusal surfaces, easily identifying the active caries.
Silver diamine fluoride from Elevate Oral Care is being used as a caries-preventive agent. It discolors demineralized tooth structure black. Additionally, it can be easily used on occlusal surfaces to allow identification of Class I caries, which turns black when the solution is placed on the occlusal surface of the tooth.
Software enhancement of current digital radiographs
Logicon caries detector software from Carestream Dental is a well-proven diagnostic adjunct for digital radiographs only for the Carestream brand of sensors.It shows the probability of the presence of a caries lesion, and it can be used on subsequent recall appointments to compare the lesions and determine if there has been progression.
Summary
The current generation of digital periapical and bitewing radiographs is considered by most practitioners to be inadequate for the accurate detection of initial dental caries. Radiographs also often obscure the presence of deep carious lesions. I encourage dentists to become more active in expressing their challenges with this problem. Inform your manufacturers and dental organizations of this deficiency in the hope that they will rectify the problem. In the meantime, consider using a few adjuncts for finding initial caries that are identified in this article.
Author’s note: Additional educational information from Dr. Gordon J. Christensen, Practical Clinical Courses:
Two-day courses in Utah
• Faster, Easier, Higher Quality Dentistry with Dr. Gordon Christensen on March 2–3, 2018
One-hour videos
• Class II Composite Resins Can Be Predictable, Non-Sensitive, and Profitable (Item No. V3554)
• Mastering Frequent Esthetic Challenges with Resin (Item No. V3582)
• Top Insurance Coding Strategies (Item No. V4783)
• Avoiding Common Administrative Errors (Item No. V4784)
For more information about these educational products, call (800) 223-6569 or visit pccdental.com.
Gordon J. Christensen, DDS, MSD, PhD, is a practicing prosthodontist in Provo, Utah. He is the founder and CEO of Practical Clinical Courses, an international continuing education organization founded in 1981 for dental professionals. Dr. Christensen is cofounder (with his wife, Dr. Rella Christensen) and CEO of Clinicians Report.