A menu for routine mandibular implant therapy
by Kenneth W.M. Judy, DDS, FAGD, FACD, FICD
While the analogy might seem far-fetched, oral implant therapy is, in a sense, dentistry's answer to Einstein's quest for a "unified theory," i.e., a set of mathematical equations that would tie together relativity and quantum mechanics. The macro-universe that we see when we gaze at the stars and beyond as well as the micro-universe of subatomic building blocks could then be understood. Einstein and his colleagues, working for the past six decades, have failed to explain how the universe works. On the other hand, over the same time period, my colleagues who have dedicated themselves to research and clinical practice in the multiple areas of implant therapy have succeeded in demonstrating to us how the oral cavity and related structures which are affected by implant therapy really work. Of course, they are to be congratulated. But a very legitimate question is, "How do these wide-ranging achievements affect my practice?"
Quite often, I find myself saying to patients at their initial consultation, "What I am proposing is not rocket science. It is easy to understand." Then we jointly look at various diagnostic materials and talk about options ... even physics and biology. Some patients say, "Doc, I trust you. Go ahead and do what you think is best for me." Others want a high level of understanding. Then I have to have a "menu," based on my education and the extent of my clinical practice. In one form or another, the same is true for all of us. To adequately demonstrate this principle and weave it into the fabric of the accomplishments we have witnessed in the field of oral implant therapy, a good place to start would be what we can offer in a structured manner to patients who are edentulous or soon to be edentulous in the mandibular arch. Most patients abhor the fact or the thought of lower dentures. Let's face it — poor function, denture pastes, facial distortion, and becoming social recluses are hardly appealing prospects for the future.
Treatment options or the "menu"
The majority, probably 90% or more, of mandibular implant cases done in the United States do not involve major bone grafts and can be treated by well educated generalists or generalist/specialist teams when required. But the keys still are education and clinical experience. If we propose a therapy menu to patients, they should be made to understand what they are "ordering," — the risks and benefits, the immediate and future costs, the number of visits, and success rates, as well as the experience of those who will be treating them. On my personal menu of treatment options are subperiosteal implants, small-diameter implants, and standard root-form implants. While there is most likely some "wiggle room" in the chart below, depending on the nature and locale of one's practice, it should serve as a beginning point for both your patients and your office auxiliaries.
Obviously, I have made a number of assumptions, but in general, the above parameters have been extremely successful in my communications with patients. What you should expect — and what does in fact exist — is a very high percentage of case acceptance. Treatment can be tailored both to patients' needs and financial capabilities. A number of cases will be utilized to demonstrate the applicability of my personal menu.
Case #1 (above) — A 20-year-old subperiosteal implant with minimum bone height and surgical extension. The patient has had no complications whatsoever. The wire-reinforced processed acrylic full-arch splint has been replaced once due to occlusal wear. It has always been permanently cemented. What the patient really enjoys is a stable posterior occlusion.
Case #2 (above) — A 20-year-old subperiosteal implant with maximum surgical extension (Misch/James design). The patient's prosthesis is an "O" ring-retained removable overdenture. Again, the patient enjoys a stable posterior occlusion. One easily resolved surgical problem occurred a few years ago, i.e., removal of a small sublingual gland. Once the patient enjoyed full function, she became fixated on trying to improve her extraoral facial cosmetics. Prosthodontic knowledge and skills are required to solve this ongoing situation.
Case #3 (above) — A 9-year-old case where four small- diameter implants were used to immediately stabilize a patient's denture. The patient had a TMD problem. The perimucosal surgery was simple and the results were immediate. It should be stressed that this technique has recently become very popular and widely used. Patients' dentures, however, should be prosthodontically acceptable before placing mini implants. Housings with "O" rings provide the retention. The "O" rings are supplied with differing levels of retention and have to be routinely replaced. (Case #3 courtesy of Dr. Alvaro Ordonez of Miami, Fla.)
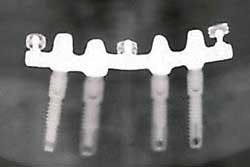
Case #4 (left) — Root form-supported connector bar with three "O" ring retention studs for patient's overdenture prosthesis. 15-year-old case with no complications. Hygiene instruction should be effective, since most patients feel that their problems have been completely solved. Implants can be placed permucosally or after surgical exposure of the alveolar ridge. Loading can be delayed or accelerated. The number of implants varies from two to five. The two implant-supported overdenture, in some circles, has become the standard of care.
Case #5 (left) — Root form implant supported fixed full-arch PFM prosthesis. Some dentists use these cases and others to advertise "same day teeth" or some catchy equivalent, and go so far as to imply that everyone is a candidate for such therapy. I couldn't be more opposed to such clinical absurdity. (Case #5 courtesy of Dr. Carl E. Misch, Birmingham, Mich.).
Case #6 (above) — After selective implant placement, extraction of teeth, and retention of other teeth, the overall "menu" can be reviewed with the patient. After a full-arch processed provisional bridge is completed, additional implants can be placed and a fixed full-arch PFM prosthesis fabricated. Copings can be used to cover the remaining teeth or they can be extracted, the sockets grafted, and additional implants placed. There are not limitless options but they should be discussed with the patient and well understood.
Utilizing the "menu" to bring a "unified theory"
New imaging technologies, new bone grafting procedures, new root form implants with varying macro and micro surfaces, and greater understanding of implant biology all can be combined with certain older technologies to generate a truly beneficial "menu" for our patients. I have limited this brief discussion to the mandibular arch. But I strongly suggest that each practitioner of implant therapy utilize the "menu" concept with their in-office team and with offices that they refer to. Then a "unified theory" will exist and bring us all to greater heights of implant therapy understanding.
Dr. Kenneth Judy is co-chair of the International Congress of Oral Implantologists (ICOI), the world's largest implant therapy society and provider of related continuing education. He is Clinical Professor in Implant Dentistry at New York University College of Dentistry, as well as in Oral Implantology at Temple University School of Dentistry. Dr. Judy has been involved in implant research and practice for more than 40 years.