Digital dentistry and its integration are also matters of customer service
Digital dentistry is not as new as some people would think. It has been a complex evolution spanning several decades. The digitalization of dentistry started in the 1960s with the development of tomography by Sir Godfrey Newbold Hounsfield and Dr. James Ambrose, a neuroradiologist from Atkinson Morley Hospital in London.1 This was followed by a thesis on optical scanning by French Professor François Duret, DDS, MD, PhD, MS, in the 1970s,2 with the first digital restoration being milled in the 1980s.3 Finally, the introduction of interactive software in the 1990s4 put the technology at the edge of popularity, only to be delayed by its expense.
Today, scanning, planning, designing, milling, and 3-D printing are realities within reach of every contemporary dental practitioner and require only an investment in resources and education.5 Adopting and integrating software facilitates communication of the devices, making the digital workflow easy and convenient.6
There are plenty of software platforms available to clinicians. Many dental manufacturers develop their own while others are under private label. When choosing a digital platform, it often comes down to personal choice and understanding which platform addresses the desired clinical priorities, such as open architecture, ease of use, integration, and efficiency.7
These criteria happen to be my benchmarks for the adoption of digital dentistry. Unfortunately, many clinicians don’t have the time or energy to do a deep dive and research which products are right for them. Going back once a decision is made can be difficult, so it is imperative to choose wisely.
Part of the selection process should involve support, as this is an essential part of any successful implementation strategy. While many issues related to digital dental devices and software can be resolved with a phone call and online support, it is critical to know who is on the other end helping.
I became involved with digital dentistry back in 1993 during my residency at Tufts University School of Dental Medicine. Our department had been part of the development process for various devices that measured bite force and occlusal contacts, muscle activity with electromyography (EMG), and jaw tracking devices. Once I was in private practice, in 2000, I adopted a popular system for scanning, designing, and milling crowns at chairside.
Fast forward to today. I am now on my fifth cone beam computed tomography (CBCT) imaging system and have owned several intraoral scanners and a number of different types of digital devices. To me, gadgets make dentistry fun and dynamic. They also keep me active studying, updating, innovating, learning, and sharing my work with dentists all over the world.
After a careful, thorough research process that included traveling to the 2019 International Dental Show in Cologne, Germany, we decided to acquire the new Planmeca Viso G7 CBCT imaging system for our practice. We were looking for a unit with a large field of view, a high scanning speed and processing time, low-dose radiation, versatility, upgradability, software integration, an intuitive platform, a good warranty program, bulletproof support, and a friendly, one-on-one customer relationship with a local representative.8
Clinically, we needed images large enough to target the full head and neck, as our practice is a comprehensive temporomandibular disorder (TMD) and facial pain center. We also provide comprehensive dental services, which include restorative procedures, implants, and endodontic work. The machine we chose would need to provide great image quality, versatility with a small field of view for my endodontist, and full head-and-neck images without multiple passes and stitching for work related to TMD and the maxillofacial area.
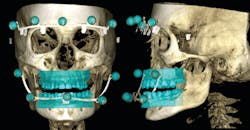
Field of view is a sensitive issue in dentistry. There are concerns related to increased radiation and liability if missing any pathology. Dentists are buying CBCT machines that have a smaller field of view to reduce radiation exposure to the patient, reduce their own liability, and reduce their investment costs.9 On the other hand, a larger field of view is required in more complex cases as is our ability to connect to the craniomandibular points of reference. These serve as landmarks to set up a proper plane of occlusion and Curve of Spee. Digitalization has left the facebow behind, which was our classic instrument of choice to create a correlation with the anatomical structures and recreate the proper plane of occlusion and Curve of Spee. As a result, more cases are now looking canted and uneven laterally or anteriorly/posteriorly.10,11 In this sense, digitalization has set us back. A limited field of view in endodontics makes sense because the doctor is targeting a small area for a specific purpose. However, when it comes to having a comprehensive image of a patient, a full craniomandibular reproduction of the different structures matters in order to create a virtual patient. In this case, less is not more; it’s actually less. A good CBCT with a facial scan and overimposed intraoral scan is just that—a virtual reproduction of every pertinent structure of the patient. What sense does it make to miss the craniomandibular points of reference when we know they need to be acquired and transferred for excellence in prosthetics? Were these points only pertinent in dental school?
The ideal situation would be to create a composite of the intraorally scanned structures with the CBCT-acquired craniomandibular points of reference to build a perfect occlusal design that involves esthetics, form, and function.
When it comes to stitching, Murphy’s Law applies. The systems tend to do the stitching at the actual point of interest. Most of the stitching I see happens at the level of the temporomandibular joint (TMJ). The TMJ is a relevant structure that requires attention in our patients. As the imaging system finishes the first pass and goes into the second, any movement—even a reduction in motion—will affect the final resolution and introduce error that will opaque the clinical concepts. A clean, crisp image is everything in our profession.
When it comes to 3-D imaging, the best images are acquired quickly and in a single scan.12 Utilizing a poor image or sending one with motion to the radiologist also sends a negative message about our practices and introduces a margin of error. This is based on my experience with my oral and maxillofacial radiologist. I had sent several images to him in which stitching raised questions related to bone remodeling or to actual motion of the image. In my opinion, it is better not to stitch.
This is what has always driven me to acquire CBCT imaging systems with bigger sensors. Part of my selection process is to evaluate technology with low radiation. Planmeca Viso G7 is a machine with extremely low radiation that allows total control of the field-of-view size, so that we acquire only what we need without losing the ability to obtain a full-size image if necessary.
In the 1980s, when I went to dental school, the field of TMJ and occlusion was very respected as gnathology ruled as a school of thought.13 Inspired by some of my professors, I sought advanced education in the field and ended up in the facial pain/TMJ/occlusion program at Tufts. The philosophy of my mentors was comprehensive, and the exams included evaluation of full-body mechanics and postural imbalances. It was impressive to conduct research on hip and shoulder mechanics and see how the EMG of the masticatory muscles and digital occlusion readings were affected by a correction of postural imbalances. The cervical vertebrae became an important part of our exam, diagnosis, and treatment with incredible results.14 As a dentist, helping patients who presented with neurological symptoms, pain, and dysfunction, which were created or worsened by dental disorders, gave me a sense of accomplishment, as I have touched the lives of many. Full head-and-neck imaging can make a huge difference in my exam, diagnosis, and treatment plan, and even in the evolution of patients’ symptoms.
This system can also do some advanced imaging that is critical for our unique needs. One is the Planmeca ProFace technology that captures a 3-D photo during CBCT acquisition, creating a virtual patient from the inside out (figure 1). Another feature I have found incredibly relevant to my work is the ability to use Planmeca 4D Jaw Motion technology. A 3-D facial photo fits perfectly in our comprehensive philosophy, since dental and occlusal form and function are major components of the facial features. The interrelation between facial features15 and each component of the occlusal scheme are better evaluated and restored in virtual models. A composite of CBCT, 3-D photo, intraoral scan superimposed on the CBCT, and mandibular dynamics provided in the 4-D jaw-tracking module allows me to replicate my patient with extreme precision (figure 2). Working on models that provide full information makes my clinical results excel. It is easy to jump from one module to the other in the integrated software, and it is simple to work within the Planmeca Romexis software platform. The potential for creating fully digital, fully functional dental prosthetics and devices is right around the corner with this technology.16,17
My patients love to see themselves in the facial scan. This is the best internal marketing tool our practice has ever had. When my patients see their own face superimposed over their skull, it’s unbelievable to them. It always prompts an engaging conversation about oral health, and it improves my case acceptance. When ready, the proposed treatment plan becomes a reality for my patients.
In my courses and lectures, I come across doctors who choose to limit volume sizes because they are concerned about the various legal aspects regarding responsibility of all the data in larger scans. I always tell them: “Don’t worry about it. Ideally, every scan should be evaluated by an oral and maxillofacial radiologist who can look at the volume thoroughly. If any pathology is detected, you have provided a tremendous service to your patient—one that is far greater than the dental service you were intending to provide.”
References
1. Petrik V, Apok V, Britton JA, Bell BA, Papadopoulos MC. Godfrey Hounsfield and the dawn of computed tomography. Neurosurgery. 2006;58(4):780-787.
2. Duret F, Termoz C, inventors: Method of and apparatus for making a prosthesis, especially a dental prosthesis. US Patent 4663720; 2010 May 5. https://patents.google.com/patent/US4663720A/en.
3. Brandestini M, Moermann WH, inventors: Method and apparatus for the three dimensional registration and display of prepared teeth. US Patent 4837732; 1989. https://patents.google.com/patent/US4837732A/en.
4. D’haese J, Ackhurst J, Wismeijer D, De Bruyn H, Tahmaseb A. Current state of the art of computer-guided implant surgery. Periodontol 2000. 2017;73(1):121-133. doi:10.1111/prd.12175.
5. Golan H. Where should you invest in technology for your practice? Dental Economics website. https://www.dentaleconomics.com/science-tech/cad-cam-and-3d-printing/article/16389692/where-should-you-invest-in-technology-for-your-practice. Published May 2017.
6. Schleyer TKL. Why integration is key for dental office technology. J Am Dent Assoc. 2004;135(suppl 1):4S-9S.
7. Birnbaum NS, Aaronson HB. Digital impression devices and CAD/CAM systems. In: Goldstein RE, Chu SJ, Lee EA, Stappert CFJ, eds. Ronald E. Goldstein’s Esthetics in Dentistry. 3rd ed. Hoboken, NJ: John Wiley & Sons Inc.; 2018:chap46:1386-1407.
8. Trava B. Understanding ROI in CBCT Technology. Compend Contin Educ Dent Suppl. 2015;1(1).
9. Friedland B, Miles DA. Liabilities and risks of using cone beam computed tomography. Dent Clin North Am. 2014;58(3):671-685. doi:10.1016/j.cden.2014.04.005.
10. Arvystas MG, Wolford LM. Establishing ideal occlusion to achieve esthetic and functional excellence: an interdisciplinary approach to functional esthetics. Compend Contin Educ Dent. 2010;31(4):288-292, 294-296.
11. Hanashima M, Sakakibara K, Slabicek R, Sato S. A study regarding occlusal plane and posterior disocclusion. Int J Stomatol Occlusion Med. 2008;1(1):27-33.
12. Santoso AP, Song KH, Qin Y, et al. Evaluation of gantry speed on image quality and imaging dose for 4D cone-beam CT acquisition. Radiat Oncol. 2016;11:98. doi:10.1186/s13014-016-0677-8.
13. Bauer A. Gnathology: Introduction to Theory and Practice. Hanover Park, IL: Quintessence; 1976.
14. Gelb H, ed. Clinical Management of Head, Neck and TMJ Pain and Dysfunction: A multi-disciplinary Approach to Diagnosis and Treatment. Philadelphia, PA: Saunders; 1977:chap2-3.
15. Hellman M. Some facial features and their orthodontic implication. Am J Orthod Dentofacial Orthop. 1939;25(10):927-951.
16. Mobilio N, Catapano S. Anatomical and Functional Restoration of the Compromised Occlusion: From Theory to Materials. London, UK: IntechOpen Ltd.; 2017.
17. Tiwari B, Ladha K, Lalit A, Naik BD. Occlusal concepts in full mouth rehabilitation: an overview. J Indian Prosthodont Soc. 2014;14(4):344-351. doi:10.1007/s13191-014-0374-y.
About the Author

Alvaro Ordonez, DDS
Alvaro Ordonez, DDS, received his dental degree from the Pontificia Universidad Javeriana in Bogota, Colombia. He continued his studies at Tufts University School of Dental Medicine in Boston, Massachusetts, where he completed a fellowship in temporomandibular joint disorder, dental occlusion, and facial pain. He was trained by Noshir Mehta, DMD; Albert Forgione, PhD; and Harold Gelb, DMD, in different techniques of conservative TMD treatment.