Managing hygiene with technology - no dentist left behind!
High-Tech Dentistry | Steven M. Seltzer
You may be surrounded by technology, and yet you still may not be enjoying a robust, profitable hygiene department because you are not managing it effectively. Using technology, combined with sound management techniques, you can improve the health of your patient population, give your hygienist a raise, and improve the profitability of your practice.
By making the hygienist responsible for a department’s financial success, doctors can raise production and practice profitability. In many dental offices, the hygiene department is broken - unprofitable and stressful for the doctor and an interpersonal challenge for most staff members.
The department’s shortcomings are often due to changing economic factors, increased government regulation, underutilization of technology, and poor or nonexistent management. After 10 years of researching and analyzing this issue, I’ve found most underperforming hygiene departments operate on a 1970s management model, adjusted only for the recent OSHA regulations and the introduction of ultrasonic scalers. A lot has happened in 25 years to make this model unprofitable.
The most significant economic factor is a dramatic rise in labor costs due to a shortage of hygienists. The laws of supply and demand dictate that costs rise during periods of scarcity. Even though the supply may have increased, hygiene labor costs in most parts of the country go up, but not down. The shortage creates imbalances that explain why hygienists earn more than some new dental graduates, twice the hourly wage of dental assistants, and a substantial premium compared to other two-year post-high school vocational programs.
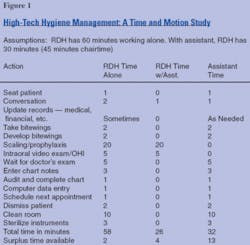
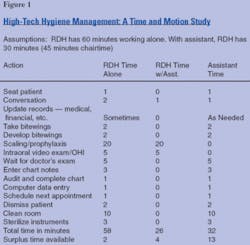
In fact, in a typical office, the hygienist spends only 44 percent of his or her time on clinical activities, which translates to more than $74 per hour for clinical functions (See Figure 1). In comparison, most dentists spend about 85 percent of their time on clinical activities.
Since reducing hygienists’ wages is impractical, doctors need to organize and manage their hygiene departments smarter. The six management actions to hygiene success are:
- Creating a hygiene profit center and empowering the hygienist with profit and loss responsibility.
- Tying hygienist compensation to profitability.
- Delegating hygiene scheduling control to the hygienist and using a computer to record procedures and schedule appointments.
- Providing each hygienist with a clinical/administrative assistant.
- Designating two treatment rooms for each hygienist to enhance productivity.
- Having the hygienist or assistant educate every patient for three to five minutes using electronic imaging (e.g., intraoral video cameras, digital still cameras).
Hygienists should be responsible for their own business areas. After all, they are highly trained and well compensated. Thus they should be viewed as partners in the practice and paid accordingly. Hygienists, like doctors, should be paid for what they do, and should not be paid for what they don’t do. The hygiene profit center matches hygiene production with expenses, and hygienists should receive a share of the profits based on performance. Production includes recall visits, deep scaling, root planing, sealants, and electronic imaging tours and X-rays, but excludes the doctor’s exam fee.
Hygienists who are paid on commission are generally happier, perform better, make more money than their salaried counterparts, and take ownership responsibility. On the other hand, hygienists who prefer an hourly wage or salary should find work at a dental practice that is willing to pay $74 an hour, as calculated in Figure 2. If you’re comfortable paying $74 an hour for a provider, perhaps you’d be better off hiring another dentist to do hygiene, amalgams, and other procedures. Practices that pay hygienists $74 an hour based on clinical work actually performed operate using a 1970s business model that assumes lower labor costs and minimal OSHA requirements.
Computer technology using point-of-treatment workstations and electronic appointment scheduling makes delegating possible. A hygienist (or assistant) who uses a chairside workstation can key in procedures performed in less than 30 seconds. She also can schedule the next hygiene visit in the electronic appointment book in less than a minute.
This approach gives her control over her schedule, reduces data-entry errors and omissions, and, surprisingly, lowers failed appointment rates. The patient appreciates the clinical necessity of the next appointment because the hygienist makes the appointment directly and motivates the patient to keep it. Hygienists who use point-of-treatment workstations say that they have more than enough time to perform these two simple tasks.
Equally important is that the receptionist, who used to enter procedures and schedule appointments, has more time to pay close attention to the doctor’s schedule, fill last minute openings, and collect money. In a typical one-doctor, one-hygienist practice - where 50 percent of patient visits are for hygiene - a receptionist has at least two extra hours a day to spend on high priority activities.
The production of a hygienist with an assistant and two treatment rooms could equal that of two hygienists with no assistants. Patients receive the same quality care and the department operates more efficiently. Data from a time and motion study presented in Figure 2 shows how an assistant, whose hourly rate is less than 50 percent of the hygienist’s rate, dramatically improves the department’s profitability.
The hygienist who works alone has 3.3 percent discretionary time (two minutes per hour) for additional patient care and other activities, while the hygienist who works with an assistant has 13.3 percent discretionary time (eight minutes per hour). Assistants have 43 percent discretionary time (26 minutes per hour) to confirm hygiene patients, fill last-minute openings, and take full-mouth series and panoramic X-rays. (Are there any outdated FMXs in your charts?)
This Seltzer Institute hygienist/assistant model is less stressful and more stimulating than a lone hygienist model. Note that it includes five minutes for an intraoral exam to educate and present the dentistry. Changing from your current system requires careful planning and some outside assistance to adapt a new system to your particular office layout and deal with behavioral issues that come with a change.
The practices which use this model have happier and more productive staffs, and the doctors have adequate time to check two patients per hour without losing productivity. Friction between front desk personnel and providers is reduced, and hygienists are less stressed and can earn more than $50 an hour. Patients are winners as well because the staff is on time and patients have more than 10 minutes per visit to talk with their hygienist and hygiene assistant.
Steven Seltzer is one of the most innovative dental practice-management consultants, inventors, and business researchers in the world. He lectures internationally, and has written more than 100 articles about practice management and technology. Seltzer developed the TLC (Technology Lighting Center) and is the founder of Seltzer Institute. You may e-mail him at [email protected] to receive an Acrobat file containing MOM’s sample content.