Midlevel dental practitioners
Gordon J. Christensen, DDS, MSD, PhD
Q: The politicians in my state are considering creating a new category of dental professional called a "midlevel practitioner." I know that similar types of practitioners are present in other parts of medicine, such as physician assistants (PAs) and nurse practitioners. Do you feel that this concept is applicable to dentistry? I'm confused with the concept and do not know how these practitioners would function in the profession.
A: All of my career, I have supported the concept of expanding the clinical responsibilities of dental assistants, hygienists, and technicians, under the supervision of a dentist. My many articles on this subject attest to that fact. However, my opinion is not unanimous. Some states and countries have legalized the expansion of clinical activities for the traditional dental team members, while others have not. Almost without exception, the concept has been successful, benefitting patients, dental staff members, the dentists working with these staff members, and the public.
What are the proven advantages of expanding the clinical activities of traditional dental team members? Among them are:
• Dentists have more time to accomplish the many clinical tasks that are legal only for licensed dentists. In busy practices this allows more patients to be treated by the dentist. If an expanded-function staff member has a clinical challenge, the dentist is there to help solve the problem.
• Staff persons involved with expanded functions have more variety in their work, which leads to more job satisfaction and a better possibility they will stay in the profession. There is no question that some dental assistants and hygienists burn out after a few years of doing the same tasks day after day. That concept is present in any vocation. Dentistry has many and varied clinical preventive and treatment procedures that can easily be shared with traditional staff members.
• Patients can be treated at a lower cost to the practice, potentially leading to lower fees to patients. Staff persons receive a salary without overhead, while dentists have a very significant overhead, recently shown by the ADA to be about 60% of total revenue collected.
• Dental team members work together under the supervision and with the help of a dentist, with each person providing some aspect of the total prevention and treatment needs, instead of being divided in different offices or geographic locations.
• There is one leader of the total team - the dentist. This highly educated and experienced person is legally responsible for all of the activities in the practice.
In summary, when you analyze the advantages of expanding the clinical responsibilities of the traditional dental team members, it is obvious that there are several winners with this concept.
While some say that midlevel practitioners are similar to expanded function auxiliaries and bring similar benefits to the profession and public, I disagree. Proponents of the midlevel practitioner state that one of the advantages is that they will satisfy the access-to-care dilemma by practicing in areas in most need of oral health-care services. This claim has been widely discussed and debated in political and clinical groups. If we assume that they will go to areas of need, what level of dental treatment is present in those areas?
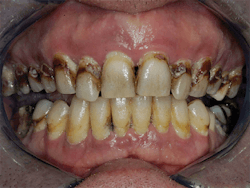
The images shown here are typical oral needs for areas of need (Figs. 1-4). Obviously, these patients require major treatment. The midlevel practitioner is supposed to treat only "simple" treatment needs. Do the patients shown have any simple needs? Can or should someone with minimal education treat these patients? No, their treatment needs stress even competent dentists.
Will the new type of practitioner elect to go into areas of need? After several decades of observing this trend in other countries, and in various forms in the U.S., in my opinion the answer is NO. I have observed and can conclude that this is a misguided and seemingly altruistic proposal usually promoted by people with minimal dental education or clinical experience.
Where do midlevel practitioners fit on the dental team? Are they assistants? No, they are supposed to be providing primary simple care. Are they hygienists? No, they are supposed to be eclectic in their services, treating overall needs. Are they dentists? No, they are not any of the above, and states where this concept has been instituted are still trying to determine where these practitioners fit in the dental team.
What is "simple" dental care? It is claimed to be simple extractions, simple restorations, emergency care, and other procedures. How many times has a "simple" extraction turned into a life-threatening nightmare, with root tips in the maxillary sinus, a heart attack, or a stroke? How many times has a "simple" restoration turned into endodontic treatment or a difficult extraction? After decades of providing oral care as a broadly eclectic prosthodontist, I am constantly reminded that prediction of simple vs. complex treatment is not easy.
What should midlevel practitioners receive as a salary? Because their role cannot be defined easily, and their education is about the level of some hygienists, there is a tendency to place their income at the hygiene level, but there is not a unanimous opinion about what to pay them. Additionally, how these practitioners will be paid is unclear. Some will work for organizations. Some will work in the offices of dentists. Some will seek administrative and educational roles. However, their level and source of income is yet to be determined.
At this time, many geographic areas in the U.S. are saturated with dentists. Where is a midlevel practitioner going to practice? Many young dentists, deeply in educational debt, and even mature dentists in highly saturated areas are unable to treat enough patients to cover their expenses. To make the situation worse, new dental schools are being initiated on a routine basis. If you contemplate this and agree with my statements, midlevel practitioners do not appear to fit into the dental team and will not go to many areas in the U.S., in spite of the need in many areas.
What can be done for dentally underserved areas? I see several obvious plans already in place in some countries.
• Federal or state funds can be diverted to build regional clinics centrally located in areas of known need.
• Dentists, especially recent graduates, can be recruited to staff these clinics for a period of time before going to other forms of practice.
• The following is a highly debated suggestion, but dentists attending low-tuition, state-funded schools could be required to spend a determined amount of time in a state or federal clinic in an area of need.
• Altruistic service groups, of which there are many, could be convinced to set up and fund clinics in areas of need as a public health service.
In summary of my long observation and opinions on this matter, adding midlevel practitioners to dentistry in the U.S. will not solve the access to care dilemma and should be abandoned as a misguided concept. In its place, dentist-supervised education of expanded duty dental assistants and hygienists should be increased and promoted by dental organizations and supported with state and federal legislation, along with immediate planning to provide other feasible ways to build and staff clinics in areas of need.
Gordon Christensen, DDS, MSD, PhD, is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Dr. Rella Christensen) and CEO of Clinicians Report (formerly Clinical Research Associates).