AI in dentistry: 7 building blocks to protect your practice
Maxwell’s demon is a term coined by computer scientist James Clerk Maxwell in 1867. The term helped him illustrate a thermodynamic experiment in which a demon controls a small massless door between two chambers of gas. Some molecules get through the door and others do not due to the demon using his tail to sort them out. In this theory, after they’re sorted, similar gases are then sorted into respective chambers by the demon’s tail toss.
Do we need a Maxwell’s demon to help us decide which artificial intelligence (AI) gets through the door of our practices and which does not? Maybe there’s a rational decision process that doesn’t involve a demon.
The best use of humans in dentistry with AI
In 1951, Norbert Wiener set the stage for machine learning (ML) and AI.1 Postulating that ML and AI could free people from repetitive tasks, he recognized the inherent dangers of computers overriding human experience. ML and AI in dentistry are becoming the norm; they intersect between computer science and repetitive clinical and administrative tasks.
I’m not worried about AI taking over our roles as dental professionals. In a 2018 paper, AI experts predicted that “human level machine intelligence (HLMI) has a 50% chance of occurring within 45 years, and only a 10% chance by 2027.”2 Whew!
Maybe ML and AI are like the Chinese symbol for crisis, both a threat and an opportunity. Let’s define the components of the Maxwell’s demon door to evaluate your opportunity with AI.
More by Dr. Margaret Scarlett
Your most strategic capital investment write-offs are in the cloud
Teledentistry: Virtual visits save time and PPE
7 building blocks to protect your practice
1. Ethics, including transparency. For now, you'll need to decide your own ethics for AI use. The World Health Organization (WHO) defined some ethical guideposts on which to build your practice. They detail six principles: autonomy, safety, transparency, accountability, equity, and sustainability.
With transparency, you balance the commercial interests of AI to ensure that the rights of patients are not subordinated. You must decide whether AI is trained with images from the diversity of populations and settings where you provide care. Basically, you need to know what AI does and does not do in a readily accessible way. This means proper labeling about how a product should be used. Be sure to read labels.
2. Regulatory issues: The Food and Drug Administration (FDA) has authority for regulating marketing claims for different AI products in the US. The FDA categorizes different classes of software for ML and AI by risk regarding what they term software as a medical device (SaMD). Class I SaMD is no or very low risk, class II is moderate risk, and class III is the highest risk if SaMD is inaccurate. However, the FDA has not decided what to do about change algorithms and transparency.
3. Marketing claims: The FDA clears marketing of claims about AI SaMD. Visit the FDA website to learn specifics about AI company applications for claims (see 510 submissions), and how much data (how many people) was used to train the computers and test their learning. Currently, these are diagnostic aids but may be actual diagnostics in the future.
4. Use cases from images now, with more in the future: Use cases are currently being designed for common oral diseases, caries, periodontal disease, and oral pathology. Radiographic images are commonly used, but because smartphones, high-definition cameras, and scanners are more accessible, a lot of information is captured that could be used for AI enhancements in the future. For now, human factors, such as caries risk assessments, are included.
5. What’s an algorithm have to do with AI? An algorithm is the formula used by the machine to perform a specific repetitive task from training data. It uses several patient radiographic images with demographic information regarding where images were taken from what patients. You will need to know this to ensure that the algorithm is relevant to your patient population.
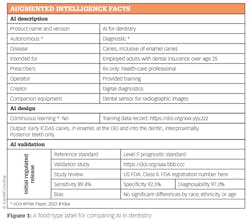
6. Labeling: The FDA requires labeling for class II and class III SaMD. Class I devices are not labeled. Many of us believe that we need simple, food-type labels that can easily compare different products, use cases, and demographics used to train the SaMD.
Figure 1 is a view of what an ideal AI label for dentistry might look like. Since most dentists do not record diagnostic codes, chief findings from medical histories, or perio risk assessments like our medical colleagues do, more innovation will happen with AI for consideration of other factors, such as the impact of the latest perio diagnostic definitions. For now, labeling images with the patient name, date of exposure, and type of image may be useful to collect for analysis of what makes sense for our practices.
7. Patient-centered care: In the absence of a clear understanding of the science and chemical and biological underpinnings of common oral diseases by the FDA, practitioners must continue to focus on patient-centered care. I could envision a research study that compared outcomes we do today versus AI-generated decisions to treat or not treat, but we don’t have data yet. This means that for now, dental professionals will be in the driver’s seat of treatment decisions.
For now, we need to listen to the “better angels of our nature” to guide our practice door guard, Maxwell’s demon. However, in the absence of that demon, dentistry will need to look toward the guideposts outlined here to engineer our own course for AI. Promising developments in ML and AI are here, with lots of work left to determine how and if humans are better than machines.
Editor's note: This article appeared in the December 2022 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Wiener N. The Human Use of Human Beings. Houghton Mifflin. Published 1950. Revised 1954.
- Grace K, Salvatier J, Dafoe A, Zhang B, Evans O. When will AI exceed human performance? Evidence from AI experts. J Artificial Intell Res. 2018;62(5):729-754. doi.org/10.48550/arXiv.1705.08807
- Ethics and governance of artificial intelligence for health. World Health Organization. June 28, 2021. https://www.who.int/publications/i/item/9789240029200
About the Author
Margaret Scarlett, DMD
Margaret Scarlett, DMD, is a dentist, futurist, and thought leader for Digital Transformation Partners. Retired from the US Public Health Service, her work centered on analysis of large population-based data sets for the Health Resources and Service Administration, the US Census for the National Health Interview Survey, the CDC for its most accurate surveillance system, and Health and Human Services. Dr. Scarlett continues to work with health systems, large DSOs, and organizations on AI in dentistry to advance digital transformation of dentistry.
Updated November 7, 2022