Teledentistry: Virtual visits save time and PPE
It’s a classic case of good news versus bad news. The good news is that dental offices across the country are now operating as essential service providers. Dentists are considered an indispensable sector of health care, which includes hospitals, nursing homes, and the practices of medical doctors. The bad news is that the COVID-19 pandemic continues across the US, spiking in certain places. Therefore, the need for enhanced infection control protocols continues, with additional personal protective equipment (PPE) recommended by both the American Dental Association (ADA) and the Centers for Disease Control and Prevention (CDC).1,2
Most practices are still wondering how their revenue will stack up in 2020, and the data says that there’s a lot of ground to make up. Beginning in March, the ADA conducted biweekly surveys that tracked key practice metrics.3 By mid-July, patient volume was at more than a quarter below pre-pandemic levels.
How can we make up the revenue? Even though we can now bill for extra PPE,4 that doesn’t fully cover additional costs or make up for lost time. The bottom line is that dental practices can’t see as many patients as before the pandemic. Solutions to address the escalating costs of PPE and extra time required are needed now.
The emergence of teledentistry
The use of teledentistry has rapidly increased in the past six months. During the lockdown and thereafter, larger group practices and dental support organizations (DSOs) quickly incorporated teledentistry into their practices without missing a beat. What did they know that smaller practices did not? Simply this: they had better ways to measure practice revenue, with managers mapping workflow for each staff member, detailing time and every duty.
Even the government is promoting telehealth. The CDC recommends that we “optimize telehealth services,”5 minimizing the risk of in-person services. Because many states have lifted restrictions on teledentistry, check with your state board of dentistry and/or state association for updates.
Assess your new workflow
We may never return to pre-COVID-19 days, but we can learn to be more efficient. In one of the offices where we practice, we started by assessing our daily workflow. We realized that we were using teledentistry as a stopgap when offices were closed, but we had not adapted it to work with in-patient care once we reopened. We asked questions such as, “What happens before, during, and after an in-patient office visit? What kind of patient education do patients need, and when is motivational interviewing used? How long and where is the patient in the office?”
With in-patient care, we weren’t seeing as many patients. We needed to be more efficient, so we looked at workflow first. This helped us choose which teledentistry platform would be best for us. Then, we incorporated teledentistry with in-patient care, which has vastly increased our efficiency.
Here’s what you need to know: Assessing workflow is a process, as well as a science. Because workflow processes are common in hospitals, we thought they might work in the dental office—and they did!
By assessing workflow, we were able to see downtime between patients, time slots that are now used for documentation or teledentistry. Instead of burning up three PPEs for hygiene checks, we got down to one. Using the CDC’s PPE burn rate calculator ensures that we never run out.6
Workflow: A closer look
For us, workflow is our map of what happens when the patient comes to the practice and what the dental team does inside the office. It includes the sequence of all physical and mental tasks performed by various people within and between the dental office. This occurs by one person, between people, and across practices (such as specialty offices), either sequentially or simultaneously.
Our office adopted a workflow template (table 1).7 For example, the workflow of ordering a medication includes communication between dentist and patient, the reasons for ordering (say, an antibiotic or a diagnosis), record keeping in the electronic dental record, and billing.For example, in our practices, the dentist writes a paper prescription, gives it to the patient or enters it into an electronic prescription, and transmits it electronically to the pharmacy. The dental assistant reminds the patient to make a follow-up appointment, and the front desk person schedules it.
Any time you make a change to your practice, especially when implementing teledentistry, the workflow associated with clinical and practice management processes will change.
Analyzing workflow for using teledentistry
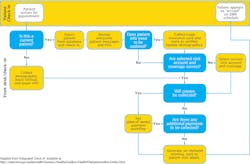
Whenever you change a process, you must assess its impact on patient care, billing, and communication. Look at the impact on the clinical side and practice management when you decide to incorporate teledentistry with in-patient care.
We were surprised to learn that many of our insurance payers now reimburse separately for teledentistry. So, we bill for teledentistry along with whatever procedures (e.g., limited oral evaluation) we perform. We have learned more about workflow in doing so.8
Our biggest front desk aha moment was how much workflow flowcharts helped us save time on patient intake. By using teledentistry, we are able to perform virtual intake encounters for patients, update medical and social histories, screen, and perform informed consent (check your state on signature requirements)—all before the visit. This saves more than 15 minutes for most in-patient visits.
The platform that we use is HIPAA compliant, both with patients and other dental specialists. We don’t spend time on emails that are not HIPAA compliant. And the front desk doesn’t have to call dental specialists multiple times to discuss the coordination of patient care.
Teledentistry has increased our workflow efficiencies. We chose the TeleDent platform (MouthWatch) because it met our clinical and workflow needs, and it has HIPAA compliant secure messaging and a smartphone-friendly patient portal. We know that our patients like to see us without PPE, especially new patients. Teledentistry makes it easier to have a conversation with them, sans masks and shields.
By using the teledentistry platform to evaluate and diagnose, we save time for both patients and our office. We estimate that about 20% of emergency patients can be seen using teledentistry. That keeps our schedule tight too.
Teledentistry can also help with coordinating care asynchronously. When multiple specialists are involved in a case, teledentistry saves about 25% on the time involved. For example, when a general dentist refers a patient to an orthodontist and oral surgeon, an asynchronous case consultation can occur. Instead of the front office chasing down the specialists, it’s easy to upload photos and 3-D images, and it’s quicker to prepare proposed treatment plans for review. Should any changes be needed, secure messaging can be used for a dialogue about treatment sequence for case completion.
The new hygiene workflow
Our biggest advantage in using the workflow analysis is in hygiene. We save about 45 minutes a day with our new hygiene workflow in addition to conserving PPE. For in-patient care, we use our new teledentistry-enabled workflow for both hygiene and restorative appointments. During hygiene visits, the hygienist provides care while wearing required PPE. During the appointment, the hygienist can capture and upload intraoral images plus notes to TeleDent.
When it’s time for the patient exam, we review radiographs and all information uploaded to TeleDent from a separate clean room. We can also choose to initiate a live video call with the hygienist, where we can view the patient through a webcam with the live feed from the on-site intraoral camera. This allows us to do a thorough exam, using teledentistry as virtual PPE. We can also choose to use the store-and-forward method, reviewing all images and notes at a later time.
By using the images the hygienist captured, we create a visual treatment plan, which is shared securely with the patient through the patient portal. Later, the treatment coordinator conducts a video teledentistry visit with the patient to discuss treatment options and scheduling.
The new restorative workflow
When planning for restorative visits, patient intake and screening are done via video calls. Our patient portal can be used to obtain consent, because the patient has already viewed the clinical photos via intraoral camera and knows the procedures that are needed from the virtual consultation. Now patients wait in their cars until we usher them directly into the operatory.
After treatment is complete, follow-up care can be done using teledentistry-enabled video calls. Patient messaging is used to answer any questions or provide postoperative instructions. Later, the asynchronous (store and forward) evaluations occur after patient care is complete, with a report sent via the patient portal. The patient receives an email saying the report is available for viewing when it’s convenient.
If the patient requests it, we will follow up with a live teledentistry visit, virtually face-to-face. We reduce in-office time by doing teleconsultations with the patient about the next treatment visit, discussing any next steps in the treatment plan. Documentation and interface with our electronic dental records are easy tasks.
Final thoughts
In the new reality of COVID-19, teledentistry allows us to schedule virtual face-to-face time with our patients, so we stay connected while limiting risks. By conducting an initial workflow analysis of our new post-COVID-19 practice, we have found that utilizing teledentistry is helping us greatly increase our efficiencies.
We’re not yet seeing the same volume of patients we saw pre-COVID-19, but we’re getting closer. Seeing emergencies using teledentistry makes our days much less stressful, and our new workflow reduces our burn rate of PPE, especially for hygiene. The streamlined approach to patient care not only saves money on PPE, it saves time too!
References
- Guidance for dental settings. Interim infection prevention and control guidance for dental settings during the coronavirus disease 2019 (COVID-19) pandemic. Centers for Disease Control and Prevention. Updated June 18, 2020, August 4, 2020, and August 28, 2020. Accessed September 22, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
- ADA releases interim guidance on minimizing COVID-19 transmission risk when treating dental emergencies. American Dental Association. April 1, 2020. Accessed July 26, 2020. https://www.ada.org/en/publications/ada-news/2020-archive/april/ada-releases-interim-guidance-on-minimizing-covid-19-transmission-risk-when-treating-emergencies
- COVID-19 economic impact on dental practices. American Dental Association Health Policy Institute. March 23, 2020. Updated August 10, 2020. Accessed July 26, 2020. https://www.ada.org/en/science-research/health-policy-institute/covid-19-dentists-economic-impact
- COVID-19 coding and billing interim guidance: PPE. American Dental Association. July 7, 2020. Updated July 22, 2020. Accessed July 27, 2020. https://www.gadental.org/docs/librariesprovider16/default-document-library/ppe_coding_billing_guidance95fc58ddb07d6e0c8f46ff0000eea05b.pdf
- Framework for healthcare systems providing non-COVID-19 clinical care during the COVID-19 pandemic. Centers for Disease Control and Prevention. Updated June 30, 2020. Accessed July 27, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html
- Personal protective equipment burn rate calculator. Centers for Disease Control and Prevention. Updated April 7, 2020. Accessed July 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/burn-calculator.html
- What is a flowchart? Agency for Healthcare Quality and Research. ASQ Quality Press. https://asq.org/quality-resources/flowchart
- Andersen B, Fagerhaug T, Henriksen B, Onsøyen LE. Creating a cross-functional flowchart. In: O’Mara P, ed. Mapping Work Processes. 2nd ed. ASQ Quality Press; 2008:61-68.
About the Author
Margaret Scarlett, DMD
Margaret Scarlett, DMD, is a dentist, futurist, and thought leader for Digital Transformation Partners. Retired from the US Public Health Service, her work centered on analysis of large population-based data sets for the Health Resources and Service Administration, the US Census for the National Health Interview Survey, the CDC for its most accurate surveillance system, and Health and Human Services. Dr. Scarlett continues to work with health systems, large DSOs, and organizations on AI in dentistry to advance digital transformation of dentistry.
Updated November 7, 2022
Eden Ivie, BSDH, RDH, PHDHP
EDEN IVIE, BSDH, RDH, PHDHP, is a MouthWatch teledentistry specialist who has been involved in the implementation of many teledentistry programs currently using the MouthWatch TeleDent platform. She can be contacted at [email protected].