Zirconia: Evolution of a unique universal restorative for anterior and posterior applications
Lee Culp, CDT, AAACD, explains how the new multilayered zirconia milling disks that offer a transition from dentin to enamel shades, along with the proper translucency differences in the areas, give the dental technician, dentist, and patient a universal restorative option for both anterior and posterior applications.
Biomaterials in dentistry must address several requirements, which include biocompatibility, strength related to intended purpose, and esthetics. The history of dental prostheses reflects a progression from function to esthetics, with gold restorations largely being replaced by porcelain-fused-to-metal restorations from the 1970s to the 1990s. The introduction of all-ceramic restorations beginning in the 1980s initiated a continuous transition from metal-based ceramics to various multilayered and monolithic all-ceramic restorations.
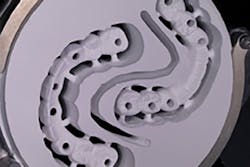
Early monolithic restoration, showing apparent opacity and high value.
The central issue for all-ceramic restorations has been balancing esthetics (color and translucency) with strength or function. Different materials have been used, and their esthetic value traditionally has been inversely related to their strength. The basis for this clinical paradox is the use of glass phase ceramics to impart translucency to dental ceramics and the use of relatively opaque crystalline ceramics to achieve strength.
Despite the esthetic limitations of zirconia-based restorations, the dental profession has seen remarkable penetration into the dental laboratory and clinical practice. The reasons for this replacement of metal and metal ceramic restorations is attributable to several factors, including the relative cost of gold alloys, the integration of zirconia materials into the CAD/CAM workflow, and the esthetic value of “white” dental materials. Suggested by this migration of clinical preferences from metal ceramics to all-ceramic materials is the satisfactory performance of the all-ceramic material.
The past decade of clinical research has provided some insight regarding the performance of zirconia prostheses. A systematic review by Raigdroski et al. looked at the survival and complications of zirconia fixed dental prostheses (FDP). He reported survival rates that ranged from 73.9% to 100% within 12 studies. Five studies reported 100% survival rates during the observation period. One study reported 73.9% survival of frameworks and the rest (six studies) had survival rates ranging between 88.2% and 96.6%. The common complication reported was chipping, and it was suggested that with the development of new layering porcelains, better clinical properties would be expected. (1)
In a second report, a 2010 systematic review on the performance of zirconia-based FDP evaluated not only the survival, but also the complication rates for this type of prosthesis up to five years. Three hundred and ten prostheses were included. The five-year survival rate for all FDP was 94.29%, and 76.41% of FDP were considered free of complications, with chipping being the most reported complication. (2) Very rarely do we see fractures within the zirconia framework itself. For example, the systematic review by Sailer et al. indicated that compared to chipping rates of 13.6%, framework fractures occurred only 6.5% of the time. (3) Observed fractures were reported most commonly in connectors of multiunit posterior restorations, and/or second molar abutments.
The systematic review of Larsson et al. in 2014 suggested that the success rate of tooth- and implant-supported zirconia-based crowns is similar and comparable to that of conventional porcelain-fused-to-metal crowns. (4) A recent laboratory study utilized indentation to induce chipping of monolithic zirconia and lithium disilicate materials. The results confirm that ceramic veneered-zirconia displayed high chipping and monolithic lithium disilicate resisted this chipping; monolithic zirconia was most resistant to this induced chipping behavior. (5)
As revealed in the aforementioned reviews concerning zirconia restoration performance, one of the early and prominent observations made regarding the clinical performance of zirconia-based all-ceramic restorations was chipping of the veneering porcelain from the zirconia frameworks. While many different investigators have suggested fundamental reasons for this phenomenon, the clinical response to chipping is a concern for layered zirconia restorations.
When used as a framework, zirconia has an inherent basic esthetic value, due to the fact that it is white and can be alternatively colored to mimic surrounding dentin. Further, it can be provided with high opacity to cover discolored teeth and implant components. (6) This can be advantageous to the technician who is trying to conceal a dark underlying tooth structure, a metal post, or the remainder of amalgam restorations left after initial preparation.
Zirconia framework-based restorations, when veneered with an appropriate ceramic layering system designed for zirconia, can result in exceptional esthetics and can achieve an imperceptible match to the surrounding dentition. The talented technician may develop appropriate color and optical properties of the restoration within the veneering ceramics. However, the past decade of investigation has revealed that chipping within the veneering ceramic or at the framework/veneer interface frustrates higher clinical success and survival of these restorations. Veneer chipping, not framework fracture, appears to be the weak link in zirconia-based restorations.
The next evolution of zirconia offers high strength and better translucency, but it still requires ceramic layering on the facial to achieve high esthetics.
Biocompatibility
Research regarding zirconia as biomaterial began in the late 1960s. Helmer and Driskell published the first paper in 1969. (7) In 1988, Christel et al. offered the use of zirconia as an alternative to other materials used at the time to manufacture the ball heads for total hip replacements. (8) Zirconia is still used in this application and other medical prosthetics to this day. Implied was acceptable biocompatibility. Clark showed that zirconia was found to be better than other ceramic biomaterials in use circa 1990 because it possessed higher strength and hardness.
The interaction of zirconia with oral soft tissues may be central to the performance of tooth and implant-supported restorations. (9) The formation of biofilm on dental prostheses—either natural tooth- or implant-supported—is material-related. A recent investigation measured the colonization of dental implant abutments. (10) DNA checkerboard analysis revealed that, compared to zirconia abutment materials, higher total bacterial counts were greater on cast or machined titanium disks after 24 hours. This confirms the work of Bremer et al. who showed that biofilm was lowest and thinnest on zirconia compared to lithium disilicate restorations. (11) The clinical impressions of low biofilm formation and limited inflammation of zirconia restorations are supported by in vitro and in vivo studies. Bacterial adhesion has proven to be slightly better than titanium. Scarano et al. reported a degree of coverage by bacteria of 12.1% for zirconia as compared to 19.3% on titanium. (12) Rimondini et al. confirmed these results with an in vivo study where ceramic material made of tetragonal zirconia polycrystals stabilized with yttrium (Y-TZP) accumulated fewer bacteria than commercially pure grade 2 titanium (Ti) in terms of total numbers of bacteria and presence of potential pathogens, such as rods. (13) It may be concluded that zirconia materials offer advantages of biocompatibility for use as endosseous biomaterials and oral biomaterials due both to their remarkable strength and durability as well as the surface properties of the materials.
Strength
Zirconia offers an excellent option for the restoration of dental implant cases. With digital design and precision milling, screw-retained monolithic zirconia (with or without facial layering) restorations can be predictably fabricated.
The introduction of zirconia-based ceramics as a restorative dental material has generated much interest in the dental profession. The mechanical properties of zirconia are the highest ever reported for any ceramic used in prosthetic dentistry. The strength of zirconia has allowed the incorporation of high-strength all-ceramics into its use for posterior FDP. (14) High strength, coupled with the possible high esthetics that zirconia offers, allows the material to become a highly valuable option in our prosthetic armamentarium.
The basis for the valued strength displayed by zirconia is its unique crystalline structure and its behavior under loads. Zirconium dioxide (ZrO2), also known as zirconia, is a white crystalline oxide of the metal element zirconium. Its most naturally occurring form is the rare mineral baddeleyite, though zirconium metal used for dentistry is obtained from the zirconium-containing mineral ore called zircon. After being processed and purified, these powders can be further processed to produce somewhat porous bodies that can be CAD/CAM-milled with great precision. Once densely sintered, a polycrystalline ceramic material is produced which, unlike most other dental ceramics, contains no glass phase.
Over the last several years, many high-strength ceramics have been developed for the construction of metal-free restorations. (15) Several studies have evaluated different all-ceramic systems and offered conclusions on where these ceramic systems may be used with success in the oral environment. Luthy et al. measured average load-bearing capacities for several ceramic systems and found 518 N for alumina-based restorations, 282 N for lithium disilicate-based restorations, and 755 N for zirconium restorations. (16) Raigrodski et al. also analyzed several different all-ceramic systems and concluded that the all-ceramic systems he studied were only to be used in the anterior, for single-crown restorations, and possibly three-unit FPDs. He also concluded that because of the higher strength of zirconia, this material offers a wider area of restorative options in the oral cavity, including posterior single units and multiunit restorations. (15)
To circumvent the need for veneering altogether, another option is to develop fracture-resistant, partially translucent monolithic ceramics. Monolithic all-ceramic restorations are becoming more accepted due to higher strength and by avoiding weak veneer-core interfaces. All-ceramic restorations—such as IPS e.max (lithium disilicate), Wieland (zirconia), and 3M Lava Plus (zirconia)—offer several all-ceramic monolithic, restorative options that have acceptable esthetics and eliminate the need for veneering ceramics altogether.
Wear
During the early 2000s, zirconia was perceived to be a material that would cause high wear to the opposing dentition. Today, this perception is being challenged. Multiple studies have shown how zirconia can be a material that is gentle to opposing dentition, compared to glass ceramics that are layered on PFM restorations. (17) This low-wear property can be attributed to zirconia’s microstructure, and its small grain size that allows for a mirror polished surface to be created that is kind to opposing enamel surfaces. (18-19)
An in vitro study by Jeung YS et al. evaluated the wear of enamel opposing zirconia surfaces. The zirconia surfaces appeared to be less abrasive to enamel than feldspathic porcelains. The study also found that polished zirconia without glazing is less abrasive than zirconia-glazed surfaces. (20) A second study by Janyavula et al. also evaluated the wear of enamel by full-contour zirconia polished and glazed. A wear simulator and producing a 4 mm slide at 20 N rate was applied and samples evaluated using a noncontact 3-D profilometer. Although the wear of glazed zirconia was more than polished zirconia, it was still less than commonly used porcelains for PFM restorations. (21)
Wear of zirconia versus enamel
These results were further investigated in a six-month clinical study that evaluated the wear on opposing dentition for monolithic full-contour zirconia prostheses. Twenty monolithic crowns were placed in patients, and mean vertical loss for specimens, antagonists, and contralateral was recorded. Both mean and maximum enamel wear were significantly different between the antagonists of the zirconia crowns and the contralateral antagonists. Under clinical conditions, monolithic zirconia crowns seemed to be associated with more wear of opposed enamel than the natural teeth, but the amount of wear was comparable to, if not less than, other ceramic systems. (22)
Esthetics
The difficulty in reproducibly achieving good esthetics with PFM restorations and the desire for metal-free solutions has led to the increased use of zirconia. The unique optical properties of zirconia require a new and different understanding of how the materials are managed. (23)
Translucency and color are important and often inseparable variables for dental restorations, and translucency may be an innate optical property of the zirconia material related to its crystalline structure.
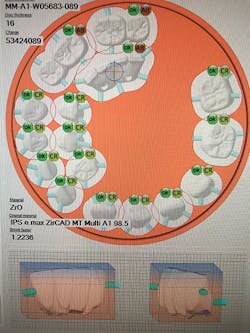
Current evolution of monolithic zirconia offers both high strength (850 MPa) and beautiful esthetics due to multiple layers of both translucency and shade within the zirconia restoration. This zirconia requires no ceramic application, as the zirconia milling disk is “prelayered.”
Conclusion
Over the past 16 years, we have seen a remarkable evolution in the esthetics of full-contour zirconia, as raw material manufacturers and ceramic companies work together to improve translucency and optical properties within this unique biomaterial. The new multilayered zirconia milling disks that offer a transition from dentin to enamel shades, along with the proper translucency differences in the areas, offer the dental technician, dentist, and patient a universal restorative option for both anterior and posterior applications.
References
1. Raigrodski AJ, Hillstead MB, Meng GK, Chung KH. Survival and complications of zirconia-based fixed dental prostheses: A systematic review. J Prosthet Dent. 2012;107(3):170-177. doi: 10.1016/S0022-3913(12)60051-1.
2. Schley JS, Heussen N, Reich S, Fischer J, Haselhuhn K, Wolfart S. Survival probability of zirconia‐based fixed dental prostheses up to 5 yr: A systematic review of the literature. Eur J Oral Sci. 2010;118(5):443-450. doi: 10.1111/j.1600-0722.2010.00767.x.
3. Sailer I, Pjetursson BE, Zwahlen M, Hämmerle CH. A systematic review of the survival and complication rates of all‐ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part II: Fixed dental prostheses. Clin Oral Implants Res. 2007;18(Suppl 3):86-96.
4. Larsson C, Wennerberg A. The clinical success of zirconia-based crowns: A systematic review. Int J Prosthodont. 2014;27(1):33-43. doi: 10.11607/ijp.3647.
5. Zhang Y, Lee JJ, Srikanth R, Lawn BR. Edge chipping and flexural resistance of monolithic ceramics. Dent Mater. 2013;29(12):1201-1208. 10.1016/j.dental.2013.09.004.
6. McLaren EA, Giordano RA. Zirconia-based ceramics: Material properties, esthetics, and layering techniques of a new veneering porcelain, VM9. Quintessence Dent Tech. 2005;(28):99-112.
7. Helmer JD, Driskell TD. Research on bioceramics. Symposium on Use of Ceramics as Surgical Implants. Clemson, South Carolina: Clemson University; 1969.
8. Christel P, Meunier A, Dorlot JM, et al. Biomechanical compatibility and design of ceramic implants for orthopedic surgery. Ann NY Acad Sci. 1988;523:234-256.
9. Bachhav VC, Aras MA. Zirconia-based fixed partial dentures: A clinical review. Quintessence Int. 2011;42(2):173-182.
10. Nascimento Cd, Pita MS, Fernandes FH, Pedrazzi V, de Albuquerque Junior RF, Ribeiro RF. Bacterial adhesion on the titanium and zirconia abutment surfaces. Clin Oral Implants Res. 2014;25(3):337-343. doi: 10.1111/clr.12093.
11. Bremer F, Grade S, Kohorst P, Stiesch M. In vivo biofilm formation on different dental ceramics. Quintessence Int. 2011;42(7):565-574.
12. Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: An in vivo human study. J Periodontol. 2004;75(2):292-296.
13. Rimondini L, Cerroni L, Carrassi A, Torricelli P. Bacterial colonization of zirconia ceramic surfaces: An in vitro and in vivo study. Int J Oral Maxillofac Implants. 2002;17(6):793-798.
14. Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008;24(3):299-307.
15. Raigrodski AJ. Contemporary materials and technologies for all-ceramic fixed partial dentures: A review of the literature. J Prosthetic Dent. 2004;92(6):557-562.
16. Lüthy H, Filser F, Loeffel O, Schumacher M, Gauckler LJ, Hammerle CH. Strength and reliability of four-unit all-ceramic posterior bridges. Dent Mater. 2005;21(10):930-937.
17. Komine F, Blatz MB, Matsumura H. Current status of zirconia-based fixed restorations. J Oral Sci. 2010;52(4):531-539.
18. Albashaireh ZS, Ghazal M, Kern M. Two-body wear of different ceramic materials opposed to zirconia ceramic. J Prosthet Dent. 2010;104(2):105-113. doi: 10.1016/S0022-3913(10)60102-3.
19. Sorensen JA, Sultan E, Sorensen PN. Three-body wear of enamel against full crown ceramics. In: 89th IADR; 2011 [Abstr. No. 1652].
20. Jung YS, Lee JW, Choi YJ, Ahn JS, Shin SW, Huh JB. A study on the in-vitro wear of the natural tooth structure by opposing zirconia or dental porcelain. J Adv Prosthodont. 2010;2(3):111-115. doi: 10.4047/jap.2010.2.3.111.
21. Janyavula S, Lawson NC, Cakir D, Beck P, Ramp LC, Burgess JO. The wear of polished and glazed zirconia against enamel. J Prosthet Dent. 2013;109(1):22-29. doi: 10.1016/S0022-3913(13)60005-0.
22. Stober T, Bermejo JL, Rammelsberg P, Schmitter M. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. J Oral Rehabil. 2014;41(4):314-322. doi: 10.1111/joor.12139.
23. Vichi A, Louca C, Corciolani G, Ferrari M. Color related to ceramic and zirconia restorations: A review. Dent Mater. 2011;27(1):97-108. doi: 10.1016/j.dental.2010.10.018.
Lee Culp, CDT, AAACD, is the CEO of Sculpture Studios, a dental laboratory, education, research, and product development center specializing in new and innovative digital dental technologies and their applications for diagnostic, restorative, and surgical dentistry. He is a leading resource and inventor for many of the materials, products, and techniques used in dentistry today, and holds numerous patents for his ideas and products.