Dental curing units, or light-curing units (LCUs), are essential in dental offices; they are used daily in restorative dentistry, orthodontics and hygiene to cure resin-based restoratives
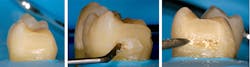
Dental curing units, or light-curing units (LCUs), are essential in dental offices; they are used daily in restorative dentistry, orthodontics and hygiene to cure resin-based restoratives, luting materials and sealants. The clinical success of all these materials depends on the LCU delivering sufficient light to polymerize the resin—otherwise, incomplete polymerization will occur (Figs. 1a-1c)
Incomplete polymerization may result in clinical failures such as bracket debonding, increased postoperative sensitivity, bulk fracture of the restoration, secondary caries because of adhesive failure between the tooth and the resin composite, and color changes within the restoration (Figs. 2a-2c).1 Having to redo such failed dental work at no charge is a recipe for financial disaster.
Although light-emitting diodes (LEDs) have the potential to last for thousands of hours, they can be damaged rapidly if subjected to a high-current density in an attempt to deliver a high light output. This can cause overheating of the LED chip and yellowing of the epoxy around the LED (Figs. 3a-3b), resulting in a reduced output of light.
Despite technological advances and the availability of LCUs that can provide a stable, high light output, most published studies show that LCUs used in offices around the world often deliver inadequate light. The dentists, however, were unaware that their lights weren't able to adequately cure their restorations.2-9
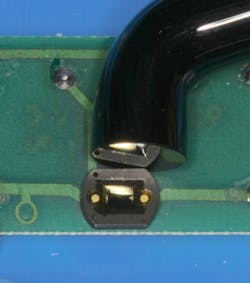
An LCU may deliver sufficient light output when new, but the light output will drop over time because the light source itself, as well as filters or reflectors within the unit, will deteriorate with use.10 Autoclaving the fiber-optic light probe can reduce the light output.11 Physical damage to the light tip and the presence of cured composite resin on the light tip are also common findings that will reduce the light output (Figs. 3a-3e).12, 13 In addition, disinfectant sprays could erode the O-rings used to stabilize the light guide, and the residual fluid could be baked onto the optics inside the housing, thus reducing the light output.14
Figs. 1a-c: Examples of incomplete polymerization. The composite is hard at the occlusal surface but soft and inadequately cured at the bottom of the proximal box.
Figs. 2a-c: Examples of clinical failures, likely because of incomplete polymerization. Note the yellow color, the debonding at the margins and the fractured resin. (Images courtesy of Dr. A. Shortall and Dr. H. Strassler)
Examples of LCUs where the optics have become damaged: overheated LED, causing bubbles and yellowing in the LED chip (Figs. 3a, 3b); damaged or contaminated light tips (Figs. 3c, 3d); and reflector damage (Fig. 3e).
Monitoring output
When using a curing light, it's impossible for the clinician to visually evaluate the quantity and quality of the light output, and the top surface of the restoration will feel hard to the touch after light curing. The combination of the intense blue light and the hard resin at the surface of restorations can provide a false sense of security that the LCU is adequately polymerizing all of the restorative material.
Thus, in view of the vital role of LCUs and their susceptibility to deliver less light output over time,15,16 every dental office should regularly monitor the output from its LCUs9 for optimal patient care and for medical/legal reasons.
Fig. 4a: Light seen through a 4.3mm-diameter entrance aperture into a dental radiometer
4b: Light tip in relationship to sensor size used in radiometer
Figs. 5a-b: The Bluephase Meter II, showing the tip diameter guide on the back of the radiometer and the irradiance recording
Limitations
The simplest and most dentist-friendly method for measuring LCU output in the office is a dental radiometer. Unfortunately, most previous studies have reported that dental radiometers cannot accurately or reliably measure irradiance from dental LCUs in mW/cm2 (light output).17-22 In fact, most dental radiometers claim an accuracy of only ±20 percent, most likely because most dental radiometers have only a narrow aperture where the light enters into the meter. As a result, different areas of high or low irradiance values may be measured depending on the position of the light tip over the aperture into the meter. Thus, the values may not represent the irradiance across the whole light tip (Figs. 4a-b).
Additionally, in some instances, the emission spectrum from the curing light may extend beyond what dental radiometers can detect. For example, Ivoclar Vivadent's Bluephase G2 and Bluephase Style deliver a wavelength of light from 385 nanometers to 515nm, and yet some dental radiometers don't measure light below 400nm or above 500nm.
Bluephase Meter II
The Bluephase Meter II is a new dental radiometer that uses a large sensor. It can measure both the power in mWatts and, when the light-tip diameter is entered into the meter, it can also calculate the irradiance (Figs. 5a-b). The manufacturer claims that this new meter can measure the power output from a curing light with an accuracy of ±10 percent, provided that the light tip is between 5-13mm in diameter.
In addition, the Bluephase Meter II can measure light from 385-550nm and report the irradiance from 300-12,000 mW/cm2. A recent study presented at the 2016 AADR meeting in Los Angeles reported that the meter met the manufacturer's specifications and could accurately measure the power from seven different curing lights tested.23
Conclusion
An easy to use dental radiometer that accurately reports the power (mW) and irradiance (mW/cm2) from their LCUs should result in more reliable curing and greater longevity of resin-based restorations. For medical/legal reasons alone, it's recommended that dentists record the power output from their LCUs when new and keep a daily record.1 They can then respond appropriately to any decrease in light output from the LCU.
Editor's note: This article was originally published in the July 2016 issue of Dentaltown magazine. Reprinted with permission. All rights reserved.
References
1. Price RB, Shortall AC, Palin WM. Contemporary issues in light curing. Oper Dent 2014; 39:4-14.
2. Al Shaafi M, Maawadh A, Al Qahtani M. Evaluation of light intensity output of QTH and LED curing devices in various governmental health institutions. Oper Dent 2011; 36:356-361.
3. Hao X, Luo M, Wu J, Zhu S. A survey of power density of light-curing units used in private dental offices in Changchun City, China. Lasers Med Sci 2015; 30:493-497.
4. Hegde V, Jadhav S, Aher GB. A clinical survey of the output intensity of 200 light curing units in dental offices across Maharashtra. J Conserv Dent 2009; 12:105-108.
5. Barghi N, Fischer DE, Pham T. Revisiting the intensity output of curing lights in private dental offices. Compend Contin Educ Dent 2007; 28:380-384; quiz 385-386.
6. Miyazaki M, Hattori T, Ichiishi Y, Kondo M, Onose H, Moore BK. Evaluation of curing units used in private dental offices. Oper Dent 1998; 23:50-54.
7. Ernst CP, Busemann I, Kern T, Willershausen B. Feldtest zur Lichtemissionsleistung von Polymerisationsgeräten in zahnärztlichen Praxen. Deutsche Zahnärztliche Zeitschrift 2006; 61:466-471.
8. Maghaireh GA, Alzraikat H, Taha NA. Assessing the irradiance delivered from light-curing units in private dental offices in Jordan. J Am Dent Assoc 2013; 144:922-927.
9. El-Mowafy O, El-Badrawy W, Lewis DW, Shokati B, Kermalli J, Soliman O, et al. Intensity of quartz-tungsten-halogen light-curing units used in private practice in Toronto. J Am Dent Assoc 2005; 136:766-773; quiz 806-767.
10. Friedman J. Variability of lamp characteristics in dental curing lights. J Esthet Dent 1989; 1:189-190.
11. Rueggeberg FA, Caughman WF, Comer RW. The effect of autoclaving on energy transmission through light-curing tips. J Am Dent Assoc 1996; 127:1183-1187.
12. Poulos JG, Styner DL. Curing lights: changes in intensity output with use over time. Gen Dent 1997; 45:70-73.
13. Strydom C. Dental curing lights--maintenance of visible light curing units. SADJ 2002; 57:227-233.
14. Strassler HE, Price RB. Understanding light curing, Part II. Delivering predictable and successful restorations. Dent Today 2014;1-8; quiz 9.
15. Pereira AG, Raposo L, Teixeira D, Gonzaga R, Cardoso IO, Soares CJ, et al. Influence of Battery Level of a Cordless LED Unit on the Properties of a Nanofilled Composite Resin. Oper Dent 2016; In press.
16. AlShaafi MM, Harlow JE, Price HL, Rueggeberg FA, Labrie D, AlQahtani MQ, et al. Emission Characteristics and Effect of Battery Drain in “Budget” Curing Lights. Oper Dent 2015; In press.
17. Leonard DL, Charlton DG, Hilton TJ. Effect of curing-tip diameter on the accuracy of dental radiometers. Oper Dent 1999; 24:31-37.
18. Roberts HW, Vandewalle KS, Berzins DW, Charlton DG. Accuracy of LED and halogen radiometers using different light sources. J Esthet Restor Dent 2006; 18:214-222; discussion 223-214.
19. Busemann I, Schattenberg A, Willershausen B, Ernst CP. Accuracy of Hand-held Dental Radiometers for the Determination of Power Output of Curing Devices. Das Deutsche Zahnärzteblatt 2008; 117:476-482.
20. Price RB, Labrie D, Kazmi S, Fahey J, Felix CM. Intra- and inter-brand accuracy of four dental radiometers. Clin Oral Investig 2012; 16:707-717.
21. Aravamudhan K, Floyd CJ, Rakowski D, Flaim G, Dickens SH, Eichmiller FC, et al. Light-emitting diode curing light irradiance and polymerization of resin-based composite. J Am Dent Assoc 2006; 137:213-223.
22. Kameyama A, Haruyama A, Asami M, Takahashi T. Effect of Emitted Wavelength and Light Guide Type on Irradiance Discrepancies in Hand-Held Dental Curing Radiometers. The Scientific World Journal 2013; 2013:7.
23. Price RB, Harlow JE, Kearns JO, Sullivan B. Power Accuracy of a New Dental Radiometer. AADR 45th Annual Meeting; JDR 2016; 95 Spec. Issue A: Abstract 412
Dr. Richard Price is the division head for fixed prosthodontics at Dalhousie University in Halifax, Nova Scotia. Price also works as a prosthodontist in the faculty practice at the university, is involved in research on implants, dental resins and curing lights, and teaches about light curing. He has written more than 100 peer-reviewed articles. In 2014 and 2015 he organized two symposiums on light curing in dentistry at Dalhousie