Instrument processing and sterilization: Key considerations
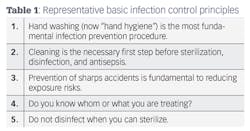
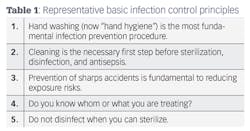
From the earliest days of their training, health-care providers (HCP) have specific infection control procedures and protocols ingrained into their daily routines. Infection prevention principles have remained basically the same over decades; a few representative ones are listed in Table 1. As advances in equipment technology and microbiology knowledge have continued to develop, however, HCP have had more choices for effectively applying these principles.
One of the more complex components of an infection control program is reprocessing instruments for patient care. It involves multiple steps, uses specialized equipment for instrument cleaning and sterilization, and requires adequate space for processing and storage. Most importantly though, qualified personnel are required to perform tasks appropriately. Continued research has also sought out more efficient ways to effectively accomplish the major components of instrument reprocessing—cleaning, sterilization, monitoring, storage of sterile items, and delivery to patients.
READ MORE | Instrument recirculation: Maximizing the process
Unfortunately, problems can arise in health-care facilities concerning how to best perform procedures for optimum results. Confusion can involve areas such as the efficacy of hand scrubbing versus mechanical cleaning of instruments, integration of instrument cassettes into practice, loading sterilizers, and monitoring sterilization cycles. This article will address a few of these key areas by using scenarios as described by clinical personnel, including the routine use of cassettes into dental practice as an increasingly important infection control component.
Consider this scenario: "Our practice purchased cassettes last year to streamline our sterilization protocols. However, there is a difference of opinion among the staff about whether prepared cassettes need to be wrapped prior to sterilization in our autoclave. In addition, one of our more experienced dental assistants insists that sterilized packages must be unwrapped, repackaged, and sterilized again if not used within six months, as she was taught in school. Is there any help to resolve these issues?"
READ MORE | Importance of instrument cleaning and cleaning monitors
Sterilization cassettes are manufactured with hole patterns that allow the sterilizing vapors to penetrate and reach instruments. When unwrapped instruments or cassettes come out of the sterilizer, exposure to the air renders them clean, not sterile—even if they go directly into drawers or cabinets for storage.
Since a long-standing infection control recommendation is to keep sterilized items free from contamination until just before use, cleaned instruments are to be packaged before being placed in a sterilizer. Selecting quality packaging material (i.e., pouches, wraps) is important, as the FDA-cleared pouch or wrap must allow penetration of the sterilization agent and also ensure that sterility of the contents is maintained during storage until use. Pouches contain an adhesive strip for sealing, while autoclave tape is acceptable for wrapped cassettes. One additional thought here is to consider where prepared cassettes and other items for sterilization are wrapped or placed in pouches. This should be done in a "clean" area, and not where dirty, contaminated instruments are set after patient treatment.
Regarding the shelf life of sterilized instruments, the guidelines from the Centers for Disease Control and Prevention (CDC) state to implement practices on either the basis of date- or event-related shelf life for storage of wrapped, sterilized instruments and devices. The event-related approach recognizes that packaged products should remain sterile indefinitely, unless some event occurs, such as packages becoming torn, wet, or punctured. Any of these occurences causes the contents to become compromised and contaminated. Instead of placing an expiration (i.e., time- related) date on packages, an indefinite shelf life label with the date of sterilization is used. If multiple sterilizers are being used, the one that was being used should be labeled with the date. An additional benefit of dating packaging is that in the event of a sterilization failure, it is easier to retrieve processed items from the specific cycles in question. Finally, whether you use time- or event-related sterilization procedures, inspect all packages just before use. If the pouch or wrap is compromised, do not use the item. The contents must be recleaned, repackaged, and resterilized before clinical use.
READ MORE | Infection Control Q and A: Instrument processing
John A. Molinari, PhD, is director of infection control for The Dental Advisor. Previously, he was professor and chairman of the Department of Biomedical Sciences at the University of Detroit Mercy School of Dentistry. Contact him at [email protected].
About the Author
John A. Molinari, PhD
John A. Molinari, PhD, is director of infection control for the Dental Advisor. Previously, he was professor and chairman of the Department of Biomedical Sciences at the University of Detroit Mercy School of Dentistry. Contact him at [email protected].
Bio updated June 1, 2017