HOW TO PROFIT from... Implants
Finally, a ‘win-win’ solution: Increasing accuracy while saving time, money with computer-milled abutments
Dental implants today have their roots in a surgical technique called osseointegration, which is defined by the American Academy of Implant Dentistry as “the firm, direct and lasting biological attachment of a metallic implant to vital bone with no intervening connective tissue.” In the 1950s, Per-Ingvar Branemark discovered biocompatibility between bone and titanium when lightweight and corrosion-resistant titanium cylinders placed in the leg bones of rabbits could not be removed because the bone had grafted itself to the titanium. This research, combined with the discovery that titanium is not recognized by the body as a foreign material, revealed that titanium is ideal for use in implanted device surgery. The first real impact of this can be seen in the world of dentistry. By 1965, commercially pure titanium was available. After Branemark’s discovery and two-stage surgical protocol, titanium was quickly accepted as the “magic metal” material of choice for dental implants. It is estimated that approximately one million people worldwide have been treated with modern osseointegrated dental implants.
During the past 30 years, the surgical aspect of osseointegration has been perfected so that dental implant survival is perhaps the highest of any orthopedic medical device. During the initial adoption of this new mode of tooth replacement, surgeons routinely placed implants “where the bone was” without a careful assessment of where the final restoration needed to be located. Since then, implant dentistry has evolved into a restorative discipline with a surgical component so that the goal of implant dentistry today is to replace the tooth. The restorative phase has undergone a huge paradigm shift, moving away from original hybrid screw-retained prostheses to morphologically shaped abutments with cemented crowns. Now implant dentistry’s focus is about how to restore the edentulous space to its most natural state, including the supporting bone, soft tissue, and emergence profile.
To accomplish tooth replacement supported by implants, the restorative dentist has three basic components from which to choose: (1) stock or prefabricated abutments, (2) custom cast abutments, or most recently (3) computer-milled abutments. Stock titanium abutments are available from many major implant manufacturers in a variety of shapes, sizes, and angulations. They are adjusted or modified manually, either at the laboratory or in the office, to adapt the shape according to the position of the implant and the patient’s individual anatomy. When there is an inadequate volume of metal for proper reduction in order to establish margin definition, antirotation, and emergence profile necessitated by patient differences in tissue height and width, stock abutments offer few options. Although many successful restorations have been fabricated on stock abutments, severe limitations exist because of the size and shape of the stock abutment. Due to a common misconception that “implants are not teeth; they have metal-to-metal contact and there are no worries about decay,” stock abutments often lack proper contours that are necessary for long-term function and esthetics. To fabricate a successful conventional ceramometal crown proper tooth reduction, 1.5-2.0 mm is required to establish margins with enough depth to allow sufficient thickness of metal and porcelain. The same applies to abutment fabrication to prevent opaque marginal porcelain or porcelain fracture, and to provide adequate translucency, strength, and overall esthetics. A stock abutment that has been inadequately prepared is shown in Fig. 1.
The next evolution in abutments was the custom cast abutment (CCA) or UCLA abutment fabricated from a plastic waxing sleeve. This sleeve was modified by the laboratory technician to establish proper contours and emergence profile. Using the lost wax method, the plastic sleeve (with or without a metal base) is invested and cast into the alloy of choice. A crown is fabricated and cemented over the post. CCAs are customized to fit the position of the implant and surrounding anatomy while allowing some degree of correction for misaligned implants. Often, I have referred to this as “prosthetic gymnastics.” A CCA is labor-intensive, can be very costly, may contain porosities in the casting, and is used mainly in the esthetic zone to control emergence profile. Its success is dependent almost solely upon the skill of the laboratory technician. In addition, there is a potential difference in fit when a totally plastic sleeve is utilized rather than a waxing sleeve with a manufacturer’s specific metal base machined to fit the specific implant. However, the UCLA custom cast abutment has been a wonderful restorative alternative that has enabled clinicians to deliver excellent results for many years.
Computer-milled abutments (CMAs) are the next evolution in abutment fabrication. These abutments are milled from a block of titanium, making them extremely strong, compatible with a specific implant, and without porosity inherent with the lost wax method. Similar to other techniques, a fixture level transfer impression is required to locate the spatial and rotational position of the implant intraorally. Once a working cast is fabricated with a soft tissue model and laboratory analogs are in place, the cast is scanned optically to generate exact 3D images of the region. This includes the location of the analog and its antirotational feature (internal or external hexagon). Through a patented process developed by Atlantis Components, Inc. (Cambridge, Mass.), one of the most current implant systems, an expert artificial intelligence system views the adjacent and opposing dentition, surrounding soft tissue levels, and implant location to design an ideal, anatomically correct virtual abutment for the edentulous space accounting for all alignment and size requirements (Fig. 2). After rigorous inspection on the computer screen, the virtual abutment design data are sent to a CNC milling machine to manufacture the morphologically correct abutment from a block of titanium alloy. The combination of 3D optical scanning methods, combined with proprietary automated expert system software and integrated machining, produces a unique abutment that conforms to a patient’s site-specific oral geometry (Fig. 3).
The move from stock and custom abutments to computer-aided design (CAD) abutments has had a positive impact on both patients and doctors, and may represent the future of abutment fabrication. What is the real benefit of a computer-milled abutment? The technology overcomes many of the obstacles that face clinicians on a daily basis. Many clinicians are intimidated by the restorative process, not knowing what parts to order, the costs involved, or what type of restoration would be best to accommodate the implant position. Therefore, laboratory technicians are faced with making decisions that - in most cases - should be made by the dentist. CMA technology greatly simplifies the process, making implant dentistry easier than conventional dentistry for the clinician. The restorative dentist needs only to take an accurate fixture-level impression, and fill out the intuitive prescription form. The opposing cast and bite are then sent directly to a dental laboratory or abutment manufacturer, like Atlantis. A morphologically correct abutment will be available for the patient at the next visit.
Because CMAs are designed specifically for each patient and account for the variations in height and rotational position, chair time and patient visits are reduced dramatically. In fact, the fixture-level impression may be the only impression required before completing the final restoration. No retraction cord, no anesthesia, no margins to capture, no porosity - just a simple transfer impression. Computer-milled abutments save valuable chair time by eliminating steps required by older methods. A typical one-hour, restorative visit can be reduced by at least 50 to 66 percent. This translates to an extra 30 to 45 minutes available for additional production time for the office.
Once the computer has the digital information that was created for the virtual abutment, why not have the CNC machines produce not just one, but two identical abutments? Using the same automated machinery (CNC milling machines) that create the CMAs, a second identical CMA abutment can be milled enabling the clinician to place one abutment in the mouth while the second abutment serves as the die for the final ceramometal restoration. Why is this significant? With a duplicate abutment in place, the restorative clinician can deliver a morphologically correct abutment and temporary that allows for proper tissue maturation. Once the tissue has matured, the laboratory technician can wax up and cast the coping directly on the duplicate abutment, ensuring accurate marginal adaptation. This is a dramatic advancement over other methods. It also improves conventional natural tooth crown and bridge prosthetics since no additional impression is required to capture the abutment shape and margin intraorally. In comparison, if a stock abutment was placed intraorally to support a similar temporary restoration and allow for tissue maturation, a secondary impression would be required to capture the intraoral abutment and then transfer this to a working cast and stone or epoxy die. Cast copings created from this indirect technique have been proven to be inaccurate due to distortions inherent in the process.
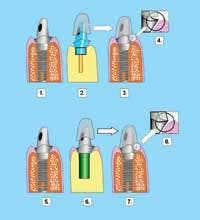
Simply stated, direct techniques are usually better than indirect techniques. An illustrative comparison can be seen in Fig. 5. The well-contoured abutment requires an impression to capture the margins (Fig. 5-1). The laboratory technician will create a die replica (Fig. 5-2) for the purpose of indirectly fabricating a cast coping (Fig. 5-3). Returning the new coping to the mouth often will result in a misfit, and large marginal discrepancy (Fig. 5-4, 5-5). These errors can be eliminated through the use of the duplicate abutment in which the coping is fabricated directly on the duplicate abutment. This results in a perfect marginal adaptation intraorally (Fig. 5-7, 5-8). Therefore, using the duplicate abutment will result in a more accurate fit, reduce the number of impressions, decrease the number of patient visits, significantly reduce chair time, lower the frequency of laboratory remakes, and virtually eliminate micromovement between coping and abutment. This results in a decrease in overall cost versus comparative methods.
While CMAs have been available for several years, many dental practitioners are not aware of the significant time and cost savings they provide. Additionally, many clinicians rely on the processes taught them in dental school (if they were exposed to implant techniques at all), and are unfamiliar with - or intimidated by - new advances in technology. More complex, multiple abutment implant restorations require a high degree of accuracy and parallelism to achieve a passive fit. These worrisome issues of parallelism and passivity are overcome by the CMA process, adding a new level of confidence for both restorative and surgical colleagues (Fig. 6). Computer-milled abutments use advanced technology to make implant dentistry easier to conduct and quicker for the patient, restorative dentist, and surgeon. This ease-of-use and efficiency combine to greatly reduce overhead, chair time, and increase accuracy and revenue - combinations any clinician can appreciate.
As conventional surgical protocols have changed since the advent of Branemark’s technique, so have restorative protocols and components. While stock abutments offer an inexpensive entry-level component, they are usually limited by their size and shape, thus preventing preparation to establish proper margins and antirotational properties. Custom cast posts were introduced to overcome these limitations and give technicians more latitude to create emergence profiles and better morphology. CCAs require that the technician create the desired shape in a wax pattern and fabricate the final post via the lost wax casting method. CCAs have been used successfully since their inception, but are limited by the extra cost, extra labor, and skill of the technician.
Computer-milled abutments have been shown to have significant advantages as compared to stock and custom cast abutments. These advantages, summarized in Table 1 (see above), include overall simplicity, reduction in the number of impressions, accuracy of fabrication, ability to create duplicate abutments, ability for accelerated treatment protocols, superior fit of copings to the abutment, significant reduction in chair time associated with the restoration phase, and a decrease in cost, especially with multiple abutments.
Scott Ganz, DMD, attended the University of Medicine and Dentistry of the New Jersey Dental School, where he is now a faculty member. He completed a specialty program in maxillofacial prosthetics at M.D. Anderson Cancer Center in Houston. An author of articles in various scientific and professional journals, Dr. Ganz has lectured internationally on implant dentistry. He maintains a private practice for prosthodontics, maxillofacial prosthetics, and implant dentistry in Fort Lee, N.J. Dr. Ganz can be contacted by telephone at (201) 592-8888, by e-mail at [email protected], or visit his Web site at www.drganz.com.
Table 1 - Advantages of Computer-Milled Abutments
- Accuracy of fabrication
- Superior fit
- Saves valuable chair time (50-66% is significant!)
- Duplicates abutment technology
- Saves even more time!
- Saves laboratory working time
- Creates a superior product
- Improved soft tissue maturation
- Increases esthetic/cosmetic result
- Time saved = money saved