How I quintupled my hygiene department in 5 years: The business of prevention
What you'll learn in this article
- How prevention-driven protocols can dramatically grow your hygiene department.
- Why hiring values-aligned team members transforms patient and practice outcomes.
- What guided biofilm therapy offers beyond traditional hygiene approaches.
- Tools and technologies that improve diagnostics, education, and patient care.
- How prevention-focused practices unlock clinical excellence and financial success.
I bought my practice in 2014. Given my commitment to preventive dentistry, my expectation was I would have an epic preventive-focused restorative practice. The reality was that I had a great restorative practice with a below average preventive practice. This dynamic is challenging for a private practice for many reasons, such as:
Restorative outcomes can be compromised: Many patients require restorative dentistry or prosthetic tooth replacement due to caries or periodontal disease. If preventive therapies are not suggested or employed, a patient is at risk for reduced outcomes or recurrence of disease.1
Patients suffer when their preventive needs are not addressed: The connection between oral health and systemic health is well-established.2 Without proper diagnosis, nonsurgical therapy, and home-care practices, patients will struggle to manage biofilm and the inflammatory process that ensues. This can exacerbate numerous systemic maladies. Our patients deserve better.
A practice cannot thrive without a robust hygiene department: Ask any practice management expert; there are specific KPIs that should be used to assess the health of a practice. These include, but are not limited to, quantifying new patients, active patients, patient attrition, and measuring the number of patients who are classified as periodontal patients.3
By 2020, I changed everything. Without realizing there was an impending staffing shortage, I decided to revamp my protocols and replace my entire clinical team. We all have our “COVID tales,” but this was the most impactful choice I’ve ever made, and I’ve never looked back.
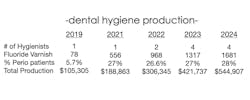
In 2023, I experienced more than a 300% growth in my hygiene department, and I shared an article about the experience.4 Since then, I’ve experienced a five-times revenue growth in my dental hygiene department in five years. I thought it was time to share how this is possible, despite a continued shortage of clinical personnel, reduced reimbursement from third party payers, and economic uncertainty.
Find the right dental team for your practice
Finding a team that is the right fit is essential. Creating a mission and vision of the dental practice will enable the practice owner to articulate what differentiates the practice and identify the practice’s core values. This is essential to attract like-minded patients and a team with similar values. A motivated team will have a profound impact on the practice’s success. If your practice is still struggling with attracting and retaining the right team, do not stop looking; they are out there!
Add guided biofilm therapy
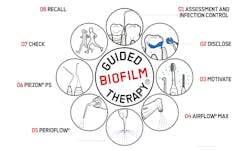
Guided biofilm therapy (GBT) is an evidence-based, systematic approach to identify and facilitate the complete removal of biofilm.5 Biofilm has been implicated in the exacerbation of dental caries, gingivitis, and periodontal disease.6 Incomplete removal of biofilm enables the maturation and colonization of pathogenic biofilm, especially in hard-to-reach areas most vulnerable to disease progression.7 GBT, a term coined by EMS Dental, involves following an eight-step compass (figure 1) within the dental hygiene appointment.
Why is this information important? Dental caries, gingivitis, and periodontal disease are extremely prevalent. There are many excellent technologies, both in-office and at-home, that are intended to combat these diseases, but the reality is that the general population is dentally and periodontally unhealthy.8
Approximately 75% of all adults have gingivitis and 20% to 50% of all adults have periodontal disease worldwide.9 Moreover, there are 57 systemic illnesses impacted by oral pathogens.10 Improving oral health can meaningfully impact the overall well-being of our communities.
Highlights of GBT
Superior patient education and engagement: The first three steps of the GBT compass allow multiple opportunities for the dental hygienist to create awareness and enhance the value of meticulous oral hygiene.11 Individualized risk assessment and home care instruction have been shown to improve patient outcomes.12 Most patients benefit from reducing hygiene intervals from six months to three to four months.13
Efficient, effective, and ergonomic biofilm and calculus removal: The system uses air-polishing devices and piezon scalers. Gentle erythritol or sodium bicarbonate-based powders are used for biofilm removal, and piezon tips are customized to enhance ergonomics and reach.
Career advancement for the dental hygienist: GBT provides a new clinical skillset and professional growth. Many hygienists certified in GBT prefer it to traditional hygiene protocols.14
A pleasant experience for the patient: Patients value the education, comfort, and advanced care involved with GBT.15
More exceptional tools for dental practices
Voice-activated periodontal charting is an exceptional tool for patient engagement. When patients are listening and educated, they often take greater ownership of their oral health. This improves case acceptance for nonsurgical procedures and specialist referrals16 (figure 2).
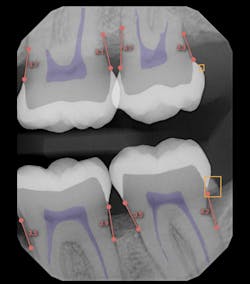
AI radiographic interpretation is gaining traction across dentistry. It helps clinicians detect pathology, guides decisions (remineralize vs. restore), and quantifies decay and bone loss for stronger third-party justification.17 AI also enhances patient education by making radiographs easier to understand visually (figure 3).
Laser bacterial removal/laser-assisted periodontal therapy (refer to state practice acts for clinical use) is good for patients with 10-plus bleeding points or who bleed during scaling and root planning. Lasers can significantly reduce the bacterial load, and this painless treatment often improves follow-up periodontal outcomes.18
Custom periodontal trays deliver a peroxide-based medicament to the base of periodontal pockets. This treatment is bactericidal and improves both periodontal status and tooth shade. Patient compliance is generally high, and results are meaningful.19
The oral cavity is part of a complex microbiome. While biofilm removal is necessary, nonspecific antimicrobials may also eliminate beneficial bacteria. Oral probiotics help rebuild a balanced microbiome that supports health and prevents pathogenic overgrowth.20
Practice management considerations
Prevention-focused protocols enhance restorative success. Periodontally healthy patients experience better results with indirect restorations and anterior esthetics.21 Hygienists are key to executing and helping these protocols evolve.
A healthy practice should reflect global periodontal disease prevalence (20% to 50%). If your metrics fall below this range, it may signal underdiagnosis. On the bright side, this also means a huge opportunity for clinical and financial growth.22
My practice saw exponential change when I hired a hygienist who is fully committed to patient wellness. Her values aligned with mine, and she implemented GBT, risk management, varnish therapy, and patient education with precision. Our hygiene team grew when like-minded, inspired professionals joined the practice, driving significant department expansion (figure 4).
Expanding the roles of dental hygienists may seem daunting to some dentists, but to others it’s a welcome challenge. A steadfast commitment to prevention not only improves clinical outcomes and financial success; it attracts top-tier talent and transforms the entire patient experience.
Editor's note: This article appeared in the August/September 2025 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Darby ML, Walsh MM. Dental Hygiene: Theory and Practice. Elsevier Health Sciences; 2014.
- Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontol 2000. 2013;62(1):59-94. doi:1111/j.1600-0757.2012.00457.x
- Levin R. The 6 critical key performance indicators for dental practices. Dental Economics. September 13, 2022. https://www.dentaleconomics.com/practice/systems/article/14207810/the-6-critical-key-performance-indicators-for-dentists
- Maragliano P. Strategies to trip your dental hygiene revenues in three years. Dental Economics. April 6, 2023. https://www.dentaleconomics.com/practice/article/14290684/strategies-to-triple-your-dental-hygiene-revenues-in-3-years
- Guided biofilm therapy. EMS Dental. https://www.ems-dental.com
- Marsh PD. Microbial ecology of dental plaque and its significance in health and disease. Adv Dent Res. 1994;8(2):263-271. doi:1177/08959374940080022001
- Van der Weijden F, Slot DE. Oral hygiene in the prevention of periodontal diseases: the evidence. Periodontol 2000. 2011;55(1):104-123. doi:10.1111/j.1600-0757.2009.00337.x
- Eke PI, Dye BA, Wei L, et al. Prevalence of periodontitis in adults in the United States. J Dent Res. 2012;91(10):914-920. doi:10.1177/0022034512457373
- Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci. 2017;11(2):72-80.
- Han YW, Wang X. Mobile microbiome: oral bacteria in extra-oral infections and inflammation. J Dent Res. 2013;92(6):485-491. doi:1177/0022034513487559
- Gehrig JS, Willmann DE. Foundations of Periodontics for the Dental Hygienist. Lippincott Williams & Wilkins; 2018.
- Chapple IL, Van der Weijden F, Doerfer C, et al. Primary prevention of periodontitis. J Clin Periodontol. 2015;42(Suppl 16):S71-S76. doi:1111/jcpe.12366
- Axelsson P, Lindhe J. Effect of controlled oral hygiene procedures on caries and periodontal disease in adults. J Clin Periodontol. 1978;5(2):133-151. doi:10.1111/j.1600-051x.1978.tb01914.x.
- EMS Dental. GBT Certification Program Feedback. Internal Report.
- Patient Testimonials: GBT Experience. EMS Dental.
- McGuire MK, Nunn ME. Prognosis versus actual outcome: a long-term survey of 100 treated periodontal patients under maintenance care. J Periodontol. 1996;67(7):658-665. doi:1902/jop.1996.67.7.658
- Schwendicke F, Golla T, Dreher M, Krois J. Convolutional neural networks for dental image diagnostics: a scoping review. J Dent. 2019;91:103226. doi:10.1016/j.jdent.2019.103226
- Cobb CM. Lasers in periodontics: a review of the literature. J Periodontol. 2006;77(4):545-564. doi:10.1902/jop.2006.050417
- Kutsch VK, et al. Peroxide gel use in customized trays for management of periodontitis. Compend Contin Educ Dent. 2012;33(7):486-489.
- Devine DA, Marsh PD. Prospects for the development of probiotics and prebiotics for oral applications. J Oral Microbiol. 2009;1. doi:3402/jom.v1i0.1949
- Avila-Ortiz G, et al. Influence of periodontal disease on the stability of anterior restorations. Compend Contin Educ Dent. 2015;36(7):494-499.
- Periodontal disease prevalence and trends. American Academy of Periodontology https://www.perio.org
About the Author
Pamela Maragliano, DMD
Chief Editor of Dental Economics
Pamela Maragliano, DMD, is the chief editor of Dental Economics. Based in Salem, Massachusetts, Dr. Maragliano began her clinical career as a dental hygienist. She went on to attend Tufts University School of Dental Medicine, where she earned her doctorate in dental medicine. She then attended the University of California, Los Angeles, School of Dental Medicine, where she became board-certified in prosthodontics. Dr. Maragliano owns a private practice, Salem Dental Arts, and lectures on a variety of clinical topics. You may contact her at [email protected].