Xerostomia relief: A different approach to treatment
Xerostomia is a common condition that frequently goes undetected. Typically associated with salivary gland hypofunction,1 xerostomia is defined as the subjective complaint of dry mouth—and it can make patients’ daily lives miserable. Xerostomia affects the ability to chew, taste, swallow, and even speak. If left untreated, it can seriously damage patients’ oral health and have a major impact on their general health. Yet dry mouth is a manageable condition, and with the right regimen, patients can live more comfortable lives.
Awareness of dry mouth’s damaging effects on oral health is rising, as the population ages and more patients seek relief for their symptoms. Dry mouth is so common that many patients believe it’s just a natural part of aging or a medication side effect that can’t be helped. They also may not understand how damaging xerostomia can be to their health. Dentists and hygienists can help patients who might be suffering in silence by offering valuable education and resources to manage their xerostomia.
Causes and prevalence
Saliva is extremely important to maintain the integrity of a healthy oral cavity. Along with other fluids, saliva functions to reduce biomass, and it is responsible for lubrication, solubilization, oral hygiene, and the initiation of digestion. It ensures an optimal mouth pH so oral functions can be carried out effectively, and it provides an array of antimicrobial and immunological components. When the quality of a person’s saliva isn’t what it should be, dry mouth poses a significant concern to his or her overall health and quality of life.2
As a symptom of certain diseases and a side effect of many medications, dry mouth impacts as much as 65% of the general population.3 The reason for its significant prevalence lies in its numerous causes, including three primary factors:
• Diseases and infection—Patients are more likely to suffer from xerostomia if they have certain medical conditions, such as autoimmune diseases, hypertension, diabetes, chronic pain, and even seasonal allergies. We know that nearly 100% of patients with Sjögren’s syndrome experience dry mouth symptoms.4 But they aren’t alone; those with other conditions may also be suffering in silence.
• Prescription and nonprescription medications—More than 700 different medications, both over-the-counter and prescription, can cause or exacerbate dry mouth.1 These include but are not limited to the drugs in the following classes: antidepressants, antihistamines, anticonvulsants, antivirals, diuretics, decongestants, and anti-inflammatory . . . to name a few. Plus, patients who regularly take multiple medications have a higher rate of occurrence.
• Medical treatment—Chemotherapy and radiation therapy for head and neck cancers devastate the salivary glands and surrounding anatomical structures. Innovative techniques in delivery of radiation and drug administration can selectively protect normal tissues and reduce the adverse effects on salivary glands. Nonetheless, patients still routinely suffer severe oral dryness.
Detection
Despite the significant prevalence of xerostomia and its related discomfort, the signs can go unnoticed by patients and professionals. Dry mouth is often a slow-progressing side effect of many conditions and medications, and most patients can’t pinpoint “when” it started. They may notice disturbances in their lives, such as waking up at night to drink water or having trouble speaking or swallowing due to low salivary flow. Yet some patients do not openly discuss their symptoms, and many do not complain about their dry mouth unless prompted with specific questions.
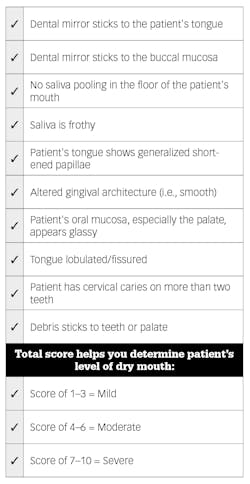
For these reasons, advocating for patients at the first signs of xerostomia can save them discomfort and prevent serious health implications. In my practice as a clinician and educator, I check for common clinical signs to identify xerostomia, beginning with a review of the patient’s medical history and an extraoral and intraoral examination, with a focus on salivary flow and palpation of the salivary glands (figure 1).
We also do our best to see dentally or medically compromised patients three or four times per year to keep a close eye on potential changes in their health. If we recognize any of the aforementioned signs, we engage with the patient to learn more about his or her symptoms and encourage taking further measures. We often see patients more than their primary medical care professionals and have a great first line of diagnostic defense systems in place to assist with this diagnosis process.
Differential diagnosis
Effective treatment planning for xerostomia begins with the initial patient conversation to gather information. As dentists and hygienists, it is our job to figure out why dry mouth is happening. We want to define the source of the issue in order to provide the most effective and personalized treatment solution. The following medical questions and considerations can help us do this successfully:
• Is the patient taking a specific type of medication that causes xerostomia?
• Is the patient’s dry mouth a symptom of a more serious medical condition?
• Is he/she undergoing radiation therapy or treatment for head and neck cancer?
• What other medications is he or she taking?
• Have any of the patient’s prescriptions changed?
• Do we need to refer the patient to a physician for further evaluation?
Given the range of possible responses to each of these questions, we could be looking at drastically different treatment protocols. A patient who is being treated for head and neck cancer, for example, will likely require a different treatment approach than a patient who is exhibiting symptoms as a side effect of a certain medication. Further discussion about symptoms can provide additional insights as we plan for effective treatment:
• Tell me about how you manage your dry mouth symptoms.
• Help me understand how that impacts you daily.
• What does that feel like?
• Are you frequently thirsty? If so, has your physician ruled out diabetes?
• Do you frequently feel a sticky, tacky sensation in your mouth?
• Have you noticed a raw, sore, or burning sensation in your mouth or on your tongue?
• Are you having difficulty swallowing? Is it more noticeable at night or at rest?
• What is the biggest frustration you have with your dry mouth symptoms?
Xerostomia relief and management
Depending on case severity, effective xerostomia relief and management is possible—and this can vary from lifestyle changes and over-the-counter solutions to prescription saliva substitutes, systemic medications, and lipid-based sprays (figure 2). Given an adequate understanding of a patient’s condition, we can offer specific treatments to help relieve dry mouth symptoms and increase the quality of life.
Lifestyle changes for mild discomfort
Patients experiencing mild discomfort and symptoms can sometimes be managed without medication through lifestyle changes that support relief. The American Dental Association (ADA) suggests sipping water or sucking on ice chips, using lip lubricants frequently (i.e., every two hours), and avoiding salty, spicy, sticky, sugary, or hard-to-chew foods. They also recommend using a humidifier at night, chewing sugar-free gum, or sucking on sugar-free mints (containing xylitol), and avoiding irritants such as alcohol, tobacco, and caffeine.
Over-the-counter and prescription-strength solutions for moderate to severe cases
Stronger preventive solutions and interventions can help ease the symptoms of moderate to severe xerostomia cases, mitigate and help prevent symptom consequences, and protect the oral environment. These include the following:
• Medications, rinses, and sprays
• In-office fluoride treatments
• Application of chlorhexidine-thymol combination varnish on root surfaces
• Sealants to pits and fissures
• Prescription-strength toothpaste
• Salivary stimulants, such as xylitol mints
New to the xerostomia relief offering is a lipid-based spray that resembles human saliva. 3M Xerostomia Relief Spray utilizes oxidized glycerol triesters (OGT)—lipids that adhere to the surface of the oral cavity—to form a protective film that moistens and lubricates the tongue, throat, teeth, and gums, while limiting water loss and restoring elasticity of the oral mucosa. The spray delivers rapid and lasting relief, without the need for mixing and rinsing. Unlike water-based products that tend to dissipate quickly, the lipid-based solution delivers clinically proven relief for up to four hours.3 Insoluble in water, the spray also provides better substantivity.
Our main objective as dental professionals is to provide recommendations that are not only personalized and effective but scientifically supported. In two clinical evaluations of the efficacy, safety, and acceptability of the lipid-based OGT spray versus a saliva substitute, participants reported that the OGT spray significantly decreased the initial severity of feelings of dry mouth, decreased initial speech difficulties, and decreased initial impaired taste.3 In vitro evaluations further demonstrated that the OGT spray protects tissue from moisture loss better than water-based products and also lubricates better than water-based products. This is a proven therapy worth considering for our patients, who deserve symptom relief and quality care.3
Bringing it all together
As dental professionals, we are often creatures of habit, recommending the same thing over and over again, not necessarily knowing if it’s really the best solution. We ought to look at what is in different products and be willing to take a chance on something new because it could be revolutionary for our patients.
Xerostomia is a manageable condition that can be treated with a range of short-term or long-term care solutions. Ultimately, effective xerostomia management depends on scientifically proven solutions and patient compliance. Helping our patients understand their xerostomia symptoms and tailoring treatment to their individual needs can benefit the relationship between patients and their dentist and hygienist, as well as their overall health.
Speaking up about xerostomia’s causes, symptoms, and management solutions can ease patients’ fears and discomfort and help protect their teeth from the harmful effects of dry mouth. Awareness facilitates a proactive approach to personalized treatment.
References
1. Department of Scientific Information; ADA Science Institute. Oral Health Topics: Xerostomia (Dry Mouth). American Dental Association website. www.ada.org/en/member-center/oral-health-topics/xerostomia. Updated July 8, 2019.
2. Braam PM, Roesink JM, Raaijmakers CPJ, Busschers WB, Terhaard CHJ. Quality of life and salivary output in patients with head-and-neck cancer five years after radiotherapy. Radiat Oncol. 2007;2:3. doi:10.1186/1748-717X-2-3.
3. Mouly SJ, Orler JB, Tillet Y, et al. Efficacy of a new oral lubricant solution in the management of psychotropic drug-induced xerostomia: A randomized controlled trial. J Clin Psychopharmacol. 2007;27(5):437-443. doi:10.1097/jcp.0b013e31814db434.
4. Lamoreux D. Finding comfort with a dry mouth. RDH magazine website. www.rdhmag.com/articles/print/volume-34/issue-3/features/finding-comfort-with-a-dry-mouth.html. Published March 11, 2014.
5. King’s College London Dental Institute. The Challacombe Scale of Clinical Oral Dryness. Challacombe Scale website. http://www.challacombescale.co.uk/Challacombe-Scale-ENG.pdf. Published 2011.
Irene Iancu, BSc, RDH, CTDP, began her career in dental hygiene in 2007 after graduating from Oxford College. She has worked in various specialties in dentistry, including pedo, perio, and orthodontics. Iancu is an international speaker, social media influencer, and clinical and theoretical dental hygiene instructor at Oxford College. She maintains a clinical practice in Toronto, Canada, with a license to practice independently. She is a key opinion leader for 3M Oral Care. Contact her at [email protected] or on Instagram (@toothlife.irene).
About the Author

Irene Iancu, BSc, RDH, CTDP
Irene Iancu, BSc, RDH, CTDP, began her career in dental hygiene in 2007 after graduating from Oxford College. She has worked in various specialties in dentistry, including pedo, perio, and orthodontics. Iancu is an international speaker, social media influencer, and clinical and theoretical dental hygiene instructor at Oxford College. She maintains a clinical practice in Toronto, Canada, with a license to practice independently. She is a key opinion leader for 3M Oral Care. Contact her at [email protected] or on Instagram (@toothlife.irene).