The case of the smoking gun
It's the ultimate whodunit case: three suspect teeth stand before you, one endodontically treated, one previously restored, and one with no prior treatment. The victim? A patient with tremendous pain and swelling that has increased significantly in just two short days. But the suspects aren't talking: traditional clinical testing and 2-D radiographs provide no smoking gun. The clock is ticking as the patient's swelling increases. You have a few hunches, as the repeat offenders, teeth Nos. 20 and 21, have a rap sheet. Tooth No. 22 has no record, so surely it's just an innocent bystander. Time is up-which suspect gets treated?
It all sounds rather dramatic, doesn't it? However, when you practice with the right technology, clinical scenarios like this one become open-and-shut cases.
Clinical case
A 33-year-old woman presented at my office complaining of pain in the lower left side of her jaw along with significant facial swelling that had started two days prior (figure 1). It was the patient's first visit to my practice and she had no significant medical history besides taking oxycodone/paracetamol (Percocet).
READ MORE | 'Hello, have you met my CBCT system?'
Diagnosis
Teeth Nos. 20–22 were examined using traditional clinical testing to determine the cause of the pain. The patient indicated that No. 20 had been endodontically treated, though she could not recall for certain the exact tooth. Diagnostically speaking, the occlusion was fine, and all other standard tests led us to believe that tooth No. 20 was not the issue.
However, teeth Nos. 21 and 22 were sensitive to both percussion and palpitation. Unfortunately, there was no significant difference in pain between the two that indicated one or the other as the cause. Tooth No. 21 had been previously restored with a large distal occlusal amalgam that was close to the pulp chamber. Tooth No. 22 appeared to show periapical pathosis; there was no thermal response when touched, though Nos. 21, 27, and 28 responded normally.
Figure 1: Different views of the facial swelling present when the patient first arrived in the office
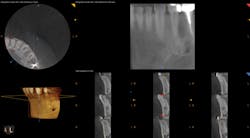
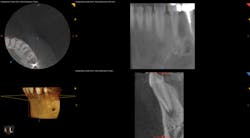
To determine whether tooth No. 21 or No. 22 was the issue, two periapical radiographs were taken. However, the results were inconclusive (figures 2–4). With clinical testing and 2-D radiographs providing no smoking gun, it was decided to use limited field-of-view CBCT (Carestream Dental CS 9000C 3D) on the region. CBCT revealed that tooth No. 22 was abscessed and a fair amount of the apical bone was completely gone (figures 5 and 6). In fact, since the time the pain began and when the patient presented at the practice, the tooth had abscessed at an alarming rate and was now considered an emergency situation.
Figure 2: A periapical radiograph showing a suspicious area (i.e., radiolucency) approximating the apex of tooth No. 20, as well as the defective distal occlusal restoration on tooth No. 21
Figure 3: A periapical radiograph showing tooth No. 22 with a radiolucency near the apex, which looked small relative to the areas on Nos. 20 and 21. There is also distortion of the appearance of the mental foramen in the area.
Figure 4: A periapical radiograph showing a partial view of the completed root canal therapy on tooth No. 22
Figure 5: CBCT showing the periapical lesion on No. 22 in multiple slices on the lower right-hand side of the image
Figure 6: CBCT showing a single view of the periapical lesion in the lower right of the screenshot
Treatment
Endodontic therapy was initiated for tooth No. 22. The pulp chamber and canal were treated with EDTA and sodium hypochlorite to help disinfect the canal system. An incision and drainage procedure was also performed to reduce the swelling and pain. A drain was placed to facilitate this process. The patient was placed on antibiotics and steroids to arrest the infection and swelling while she continued to take pain medication as needed. After five days, she was seen again in the office for removal of the drain. Two days later, the patient came in, the canal system was disinfected, root canal therapy was performed on tooth No. 22, and the tooth was successfully restored. The patient was most grateful for the quick, accurate diagnosis and treatment that reduced her significant facial swelling, and more importantly, relieved her of tremendous pain.
Conclusion
Without a CBCT system and with inconclusive radiographs, this case could have gone one of two ways. With no clear smoking gun, I would have been forced to choose between No. 21 and No. 22, hoping that I chose the correct tooth, or I could have adopted an aggressive approach and treated both. Once I would have drilled into the pulp chamber of one of these teeth, there would have been no going back-whether I had made the right decision or not. I also could have gone the wait-and-see route or referred her to a specialist; in either case, I would not have been providing immediate diagnosis or treatment. This would have proven disastrous for the patient given how quickly the tooth abscessed and most likely would have landed her in the emergency room or with a much less favorable outcome. Fortunately, CBCT clearly revealed the culprit.
READ MORE | Why I bought a CBCT system as a general dentist
I've since presented this case to the residents at the local hospital where I teach and asked for their opinions. They gave the standard answers: check for bite-related issues, etc. From a teaching perspective, this case has proven to be valuable in demonstrating the importance of CBCT for the general practitioner. I find it critical in making accurate diagnoses for difficult cases and providing enhanced treatments. The woman in the case above was a first-time patient; desperate Internet searches over the weekend for a dentist had led her to my practice. Without CBCT, I may have simply referred her out and her search would have continued. Instead, I was able to make a confident diagnosis and provide the relief the patient was looking for. Case closed.
Jay Cazes, DDS, FAGD, is a graduate of the Georgetown University School of Dentistry. He owns a practice with his wife, Janice Cazes, DDS, in Long Valley, New Jersey. Offering a number of services, such as implant dentistry, endodontics, and orthodontics, Dr. Cazes relies on CBCT when diagnosing and treating patients.