How cone beam technology revolutionized my practice
For more on this topic, go to www.dentaleconomics.com and search using the following key words: digital radiology, cone beam computerized tomography, 3-D, dental imaging, implantology, TMJ, panoramic radiography, oral pathology, treatment-planning, stealth implant surgery.
Technical advances in dentistry are occurring at an exponential rate. Dental radiology has undergone radical technological shifts in the last 30 years. During that period, we have gone from the dip tank to automatic processing to panoramic to digital radiography. We have now arrived at the 3-D revolution with cone beam computerized tomography (CBCT). Since its arrival in the 21st century, 3-D diagnostic software and CBCT have set new standards in dental imaging.
Despite these advances, the majority of dentists in North America do not yet routinely utilize CBCT in diagnosis and treatment-planning when evaluating dental, orofacial, and temporomandibular joint problems. For dental practices, the question now is whether to embrace the new technology by purchasing a system, start up an imaging stand-alone laboratory service, or establish a CBCT lab.
I became completely convinced about the CBCT revolution through evolution. I graduated from the University of Detroit School of Dentistry in 1981. Soon after starting practice with my father, Dr. Lawrence Lark, in Ida, Mich., a small farming community, I became interested in two emerging dental special-interest areas: temporomandibular joint disorders and implantology.
In that era, we made use of a 286 MHz Microsoft PC with a five-megabyte hard drive using the DOS operating system for $50,000. We purchased an additional 10 megabytes for $10,000! We were off and running in the information technology age.
As with most offices of the day, we employed many of the accepted radiographic techniques: panoramic, lateral and AP cephalometric analyses, and transcranial radiographs. Image quality and distortion from superimposition of structures was often an issue. But we were practicing dentistry with “state-of-the-art imaging.”
Brief history of dental imaging
To understand the many benefits of CBCT, it would be helpful to briefly review the recent history of commonly used dental imaging modalities before the advent of CBCT. Prior to CBCT, we had confidence in our radiography, but we now realize there was a lot of educated guesswork used when making clinical decisions with the aid of only periapical, bitewing, and panoramic radiographs.
Implantology before CBCT
Implant-planning was done with templates derived from using arbitrary magnification ratios to interpolate implant-site acceptability using periapical radiographs and panoramics. These films yielded no information about the buccal-lingual aspect of bone availability, the bone contours, nerve or sinus position, or bone density. Indirect techniques measuring stone casts were used to estimate the width of bone and location of the mandibular lingual concavity. Plane-film mandibular, panoramic implant-site analysis is fraught with potential error.
Temporomandibular disorders before CBCT
Transcranial temporomandibular joint films were popular in the 1980s, but were soon exposed by researchers because they showed a distorted view of the lateral pole of the mandibular condyle. In the late '70s, Dr. Arthur Quint developed the “Quint Sectograph,” which offered the improved cephalometrically axial-corrected TMJ tomogram. Using a submental vertex, geometric equations were employed to calculate the exact angle of the long axis of the mandibular condyle. The Quint technique created a much better image of the TMJ, but it was radiation intensive, took an hour to complete, and was limited to condylar form and position in the fossa. This was dentistry's first exposure to 3-D, but it had limited diagnostic value. Hospital-based hypocycloidal TMJ tomography was also available, but it was not dentist-friendly.
Limitations of panoramic radiography
The panoramic radiograph offered a flat-map view of the maxillo-mandibular complex, imaged by passing and elliptically moving the X-ray beam and target film plate around the patient's head. Panoramic radiography offered many new dimensions. It was able to scan the entire maxillo-mandibular complex for gross pathology and dental charting at a glance. It opened the window to radioopacities and radiolucencies. It revealed impacted tooth positions, fractures, relative superior-inferior position of the maxillary sinus and mandibular nerve canal, and permitted us to obtain a generalized sense of periodontal status. It also served as an excellent forensic record of missing and filled teeth.
However, distortions related to the radiographic trough and beam-intersection angle created unreliable magnification and vague views and dimensions of the mandible, the maxilla, and the condyles. Tooth sizes can vary greatly depending upon their relationship to the focal trough. Panoramic radiography was not accurate enough to obtain a full appreciation of the patient's anatomy.
Panoramic was not acceptable for implant treatment- planning because irregularities and distortions did not allow accurate evaluation of vital structures such as the nerve canal, floor of the nasal cavity, and maxillary sinuses. The use of implant templates to plan the size and position of implant placement was imprecise due to distortions in magnification and asymmetry of panoramic radiographs.
Traditional in-office radiographs
Periapicals and bitewing radiographs were and still remain the gold standard in detection of alveolar bone levels and caries. However, it is difficult to show superimposed canals or track endodontic infections with parallel or angled periapical films. Digital radiography has decreased radiation exposure from routine dental-detection films, but it is of limited use for determining the third dimension of dental alveolar disease.
Oral maxillofacial treatment-planning
Oral surgeons and orthodontists have used a myriad of radiographs to plan comprehensive maxillofacial orthodontic/orthognathic treatment-planning based upon 2-D images of 3-D anatomy. Orthodontic cephalometric norms have been traditionally established using a 2-D cephalometric analysis of a 3-D dentofacial complex, and relying on study models and AP cephalometrics to fill in the missing holes. Information concerning the available buccal plate, condylar asymmetry, and dentofacial growth disturbances may have been overlooked since there was no reliable means of marking and measuring the growth data.
Limitations of medical CAT in treatment-planning
In the '80s and early '90s, oral maxillofacial surgeons were taught that the standards for diagnosing trauma were the Water's, Town's, submental vertex, occlusal, panoramic, and transpharyngeal views. It was not until the emergency rooms began using medical computer axial tomography that we had more reliable imaging for determining the extent and anatomy of facial trauma. Tracking the source of infection was improved with CAT scans. However, hospital CAT centers were difficult to utilize for dentofacial needs, since medical imaging did not address dental terminology and the medical software applications did not closely align with the diagnostic requirements of dentistry.
When assessing approaches to impacted teeth, it is difficult to determine the exact position of the mandibular nerve in relation to the roots. It is also difficult to ascertain the position and direction of unerupted teeth prior to orthodontic-exposure surgery.
Magnetic resonance imaging ushered in the next advance in dental imaging, allowing us to actually see images of the soft-tissue components, such as disc, muscle, and inflammatory and infectious infiltrates. MRI has all but replaced arthrography for disc imaging. Though MRI exposed the patient to no radiation, it poorly imaged bone and was not reliable for diagnosis of fractures, osteoarthritis, or developmental skeletal disturbances.
MRI could be used for soft-tissue pathology such as disc problems, tumors, and effusions, but gave inconsistent information regarding bone pathology. And the average fee for an MRI was $1,000.
Why guess when you can know?
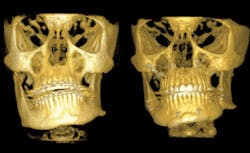
In the new century, dentistry has entered the era of cone beam computerized tomography. CBCT scans a 3-D volume of the entire head through the use of sophisticated, but user-friendly software. It allows us to evaluate, diagnose, and formulate surgical, orthodontic, and restorative treatment plans based upon accurate and precise measurement of skeletal structures. CBCT exposes the patient to five to 20 times less radiation compared to medical CAT of the same structures. CBCT does not render soft tissue as well as medical CT, but it is more than adequate for dental applications.
Oral pathology and trauma
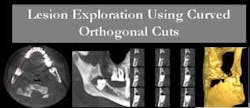
If my practice was to join the 21st century, I felt that I could no longer be tethered to superannuated imaging technology. CBCT allowed me to view previously hidden conditions. It allowed me to observe and precisely measure pathology and to do serial tracking of expanding or contracting lesions. Tracking the road map of infectious lesions became more predictable in 3-D. Volumetric stereolithic models aided in the surgical planning of oral maxillofacial plastic reconstruction after trauma or cancer surgery.
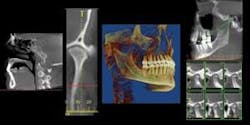
Software designed to display serial sections of the bilateral temporomandibular joints in the sagittal, coronal, and axial projections offers complete spatial-imaging capability. Visualization of cortical degeneration, cyst formation, and condyle fossa position becomes simplified. The digital ruler allows exact measurements of ramus height, condylar volume, and surface. The occlusion and dentofacial data can be observed using a 3-D volume-rendering application.
CBCT offers a method to measure developmental norms in facial and craniomandibular growth. Three-D volume rendering gives a calculable means to observe joint-based occlusal shift from temporomandibular joint disorders. Specialized orthodontic software melds 3-D photography with the CBCT scan, allowing the orthodontist to better evaluate the role of the skeleton and tooth position in creating acceptable dentofacial esthetics.
The American military is now using CBCT to archive the anatomy of soldiers' heads prior to entering the theater of combat. If a head or jaw injury occurs, CBCT stereolithography and surface-rendering allow reconstruction of a facial and skull scaffold to perform reconstructive surgery and tissue-engineering.
Prosthetically-driven stealth-implant surgery
CBCT enables us to plan prosthetically-driven, stealth-implant surgeries and operate predictably within safe-zone parameters. CBCT allows us to evaluate bone density to aid in the treatment-planning of implants, and to offer a new window into the quality of bone as related to pathologic conditions. Stereolithic models are helpful when planning bone-borne surgical guides.
CBCT allows us to evaluate sinus health and exact dimensions prior to performing subantral implants or sinus-augmentation procedures. Treatment-planning preimplant ridge-bone augmentation requirements permit more predictable implant placement. The stealth implant surgery guide allows the surgeon to correctly place implants through a low-invasive tissue punch access, thus eliminating the need for large surgical flaps. This decreases the risk of infection and suture-line opening. It also decreases time.
Airway analysis
CBCT can be utilized to calculate the 3-D volume of the oropharyngeal airway. This is important when diagnosing and treating upper airway resistance problems, as well as pretesting the effectiveness of oral-advancement appliances in the treatment of obstructive sleep apnea and snoring. There are third-party programs being developed which will be able to calculate the exact airway volume in cubic centimeters and compare pre-and post-treatment recordings.
The decision to purchase CBCT
The tipping point in my decision to purchase a CBCT unit came when I was planning the design of my new office. I had to make a decision regarding the future of imaging in my new building. I needed to know which imaging systems would best support the future of the practice.
The procedure mix in my practice needed a radiology department which supported prosthetically-driven stealth-implant surgery treatment-planning, oral pathology and infection-tracking, growth and development of the skull and mandible, airway assessment, caries and periodontal evaluation, trauma triage, and staging of surgical approaches to third-molar impactions and supernumerary teeth.
The i-CAT CBCT provided solutions to all of these needs except periodontal disease and caries detection. To meet our dental alveolar needs, we purchased the Scan–X® phosphor plate system.
I obtained a trial version of the i-CAT software and test drove it for about a year as I designed the new office. It became immediately apparent that the value of this technology was much more than what was advertised.
The 3-D software allows the user to perform 3-D virtual dissection of the head and upper cervical spine to help delineate pathology. The target areas can be rotated and flipped to gain optimal viewing angles. JPEG and PDF captures make sharing information very simple.
The implant-planning software, Virtual Implant Placement (VIP®), lets me virtually plan each implant case in 3-D, and have surgical guides fabricated to plan stealth-implant surgery to a zone of safety for vital structures. Diagnostic wax-ups of the prosthetic area help to visualize available bone relative to the desired tooth replacement. Implants are placed where the teeth need to be, not based solely upon where there is available bone. This technology lets me plan where to place the implant for proper occlusal relationship, and augment the bone where the implant-crown complex is desired. Specific implants can be ordered after planning, thus decreasing the need to have an overstocked implant inventory.
CBCT does have a few obstacles, such as metallic scatter, potentially large data file sizes, and an operator learning curve. As software applications improve, these potential problems are diminishing.
In addition to the i-CAT, cone beam technology is available from NewTom Dental (NewTom 3G and VG), Sirona (GALILEOS), Planmeca (ProMax CBV 3D), Kodak/Imtec (ILUMA), J. Morita (3D Accuitomo), TeraRecon (Dental CBCT), Hitachi (CB MercuRay), Siemens/Philips/GE (MDCT), and Gendex (GXCB-500). Many of these devices are photographed in Figure 2.
Staff and patient reaction
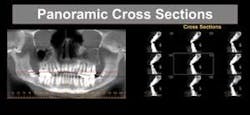
I decided to invest in cone beam technology when I realized that conventional dental images did not satisfy the diagnostic demands of implant, TMD, and orofacial pain in treatment-planning. It became apparent that 2-D imaging offered only a limited window to visualize pathology, and a less-than-precise method for treatment-planning implant placement. The CBCT allows for multi-plane reconstructions, encompassing all of the traditional radiographic plane views and mandibular or maxillary panoramics, with the additional bonus of allowing cross-sectional cuts. Cross sections offer the diagnostician access to the third dimension.
There are few times in a practice lifetime where we can be integral to a paradigm shift in the delivery of dental care. My staff was excited about being trained in cutting-edge technology. Even though the computer information-management software looked daunting at first, we all mastered the basic programs within a few days. When we installed the i-CAT, we involved our referring oral surgeon in the training so he could learn the benefits of CBCT. He is now our No. 1 referral for scans.
Patients are amazed when they see their skull being rotated and examined. The experience gives them a sense of a detailed caring for their needs. Most have never been exposed to such a thorough radiological inspection. Our patients are e-mailed JPEGs or PDFs of their images, and often engage in “show and tell” with friends and family. This type of free word-of-mouth exposure is positive for the practice.
As the number of CBCT installations increase, more dentists will become familiar with diagnosing in the 3-D environment. As software improves, cone beam will offer advanced capabilities in the areas of biomimickry, reconstructive trauma surgery, and tissue engineering.
Through the entry of computer-savvy young people into the dental profession, the updating of dental school curricula, and the word-of-mouth endorsement of dentists, I predict that within 10 years, either directly or indirectly, CBCT will be used by all dentists. Why? Simply put, CBCT improves our diagnostic capabilities and assures that we can better care for our patients.
In future issues, Dr. Lark will write more about cone beam technology in the article “Technical Overview — Scientific,” “Capabilities and Applications,” and “ROI on Cone Beam Business Plan.”
Matthew R. Lark, DDS, MAGD, FICD, FACD, has practiced general dentistry in Toledo, Ohio, for the past 26 years. He is the current president of the American Academy of Orofacial Pain. He is also an assistant clinical professor at the University of Toledo Medical Center, Department of Dentistry and a clinical instructor at the Kois Center. Dr. Lark is conducting clinical research using cone beam radiology as a diagnostic aid for implantology, orofacial pain, head and neck pathology, and sleep disorders. You may contact Dr. Lark by e-mail at [email protected].