Buyer beware: The lowdown on 8 budget curing lights
Authors
Alia Osseiran, MPH, MS
Richard B. Price, DDS, MS, PhD
Katie Dunn, MAT
Duong Tran, DDS, MPH, PhD
Cristiane Maucoski, DDS, MS
Gerard Kugel, DMD, PhD
Light-cured resin-based composites (RBCs) have become the material of choice for anterior and posterior direct restorations. Unfortunately, a Cochrane review published in 2021 concluded that direct RBC restorations placed in posterior teeth have almost double the failure rate of amalgam restorations.1
The gingival margin of class II RBC restorations is the most prevalent site for new caries formation.1,2 This area is farthest away from the light tip, and it may be in a shadow due to the angle of the light tip over the RBC.3-5 Additionally, when RBCs are inadequately photocured, they are more likely to leach undesirable chemicals into the mouth.6-8
Therefore, it is crucial that the dentist purchases a good light-curing unit (LCU) and then uses it correctly.9-11 Other factors such as the design ergonomics and the ability to access all parts of the mouth with the light tip,9,12-14 and the effects of battery discharge15-17 on the light output should be considered.
The problem with online marketplaces
Good LCUs from major manufacturers are expensive, and dentists may purchase their LCUs from an online marketplace. At least 11% of the dental supply market has shifted to online sources.18
How do I know if a device is FDA approved?
In the United States (US), the Food and Drug Administration (FDA) Code of Federal Regulations Part 87219 classifies LCUs as medical devices. Before any medical device can be used on patients, it should have received approval from the FDA.20,21
The FDA provides a guide24 and a database of medical devices that they have cleared or have received 510(k) approval.25 If a device cannot be found on the FDA website, you can ask the manufacturer for a copy of the product's 510(k), or submit a query to: [email protected].
It is up to the purchaser to determine if an online purchase has been FDA approved and can be safely used on their patients. Although the purchaser may think online sellers check to make sure their products comply with all laws and regulations, in reality, the FDA has found that the filters used are often inadequate.22 In addition, at least one major web-hosting company states that they take no responsibility for the products they sell.23
Since most researchers only use LCUs from major dental manufacturers, this study evaluated the light output from eight brands of budget LCUs purchased from online marketplaces and one LCU from 3M. The hypotheses were that:
1. The budget LCUs purchased online would have a lower power output than the LCU purchased from a major dental company.
2. The light output from the budget LCUs would not remain stable as the battery discharged.
The testing
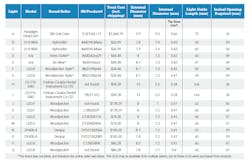
To test budget LCUs that had been made at different times, this study purchased two examples of each of the budget LCUs at two different times. Some lights could not be identified as they shared the same serial number. See Table 1 for extensive information about the individual LCUs.
The LCUs were used 500 times for 20-s (2.8 hours). They were recharged after every 100 light exposures (2000-s of use). The mean radiant power, coefficient of variation in the power values, the mean irradiance, beam profiles and ergonomics of the budget LCUs were compared against one LCU from a major dental manufacturer.
Light size and power
Table 1 shows that, in general, the budget LCUs had small internal diameter light guides that ranged from 5.4 to 7.4 mm (area 23 mm2 to 43 mm2). In contrast, the inner tip diameter of the LCU from the major dental manufacturer was 9.2 mm (area 66 mm2).
Since the irradiance is a value calculated from the quotient of the power and the area,26 the only reason these budget low-power lights delivered an irradiance above 900 mW/ cm2 is because they have a small light tip. To clarify, reducing the tip diameter from 9.2 to 5.4 mm changes the tip area from 0.66 cm2 to 0.23 cm2. This means that the LCU with the smaller tip need only deliver 34% of the power to deliver the same irradiance as the LCU with the larger diameter tip.
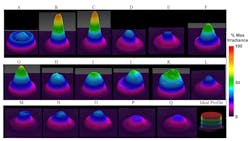
This fact illustrates the problem of using an averaged tip irradiance value. The beam profiles also showed that a single irradiance value cannot describe the output from the LCU. Figure 2 illustrates that LCUs with these small diameter light tips do not cover an entire MOD restoration in a molar tooth with an even amount of light. Instead, it would require multiple exposures from different locations to fully cover the RBC with light.
If the dentist were to use an LCU with a small diameter tip and does not deliver additional exposures over each proximal box and relied instead on a single exposure at the center of the restoration, they would likely deliver insufficient energy to fully cure the RBC.4,5,12,13 This is likely to be one of the reasons why the gingival margin of class II RBC restorations is the most prevalent site for new caries formation.1,2,10
User frustrationsWhile the user-friendliness of each light is challenging to express in standard laboratory measurements, the authors noted several issues with the LCUs purchased from online marketplaces:
- Multiple clicks of power button required to turn on light, even after as few as 10 exposures
- In the second half of the 100-exposure cycle, some lights required additional resting time and clicks of the power button, indicating that the LCUs were overheating
- Lack of indication that the light was fully charged
- Failure to charge fully
- Easily displaced from charging position
Although all lights tested had a low battery indicator, Light K continued to function while indicating a low battery but at a decreased power output. This produced a substantial standard deviation (+ 262 mW) and coefficient of variation (0.3) in its power results.
In contrast, the light from 3M exhibited a very low standard deviation (+ 8 mW) in its power results and a low coefficient of variation (0.01), which was 30 times less. The human eye cannot readily detect changes in the light output from the LCU, and apart from problems with the charger in unit K, all the LCUs produced the same bright blue light to the human eye. This loss of the radiant power over time indicated that the clinicians should periodically check their LCUs9,30 using an accurate dental radiometer such as the Bluephase Meter II.31,32
Beam profiles
Testing found that the 2-D and 3-D beam profiles show the irradiance is not uniformly distributed across the light tip and would not cover an extensive MOD restoration in a molar tooth (figures 2 and 3).
Beam profiling requires expensive equipment and cannot be performed in a dental office. Good manufacturers design their LCUs to deliver a relatively uniform light output across the light tip that will cover a molar tooth, and they will often report the beam profile from their LCU. However, the same cannot be said for the manufacturers of budget lights that did not perform as well.
Positioning
The high power or irradiance values measured on the laboratory bench mean nothing if the light tip cannot be correctly positioned over the RBC. In such locations, the light-curing may be suboptimal when these LCUs are used due to the difficulty in positioning the light tip perpendicularly over the posterior restoration.4,5,12,33
Many of the budget LCUs were awkward to use, and the patient would have to open as much as 65 mm at the incisors to fully access the occlusal surface of the second molar (figure 4). When the average mouth opening is reported to be 43 mm for males and 41 mm for females,34 only Lights A, H, and I would allow full access to the second molar.
While Lights H and I had small incisal to incisal edge-to-edge opening, the internal diameter was only half the size of the external diameter of the light guide tip. This made it difficult to accurately tell over which part of the tooth the light was positioned. This could result in suboptimal curing when using Lights H and I.
Costs in time
Although the dentist can compensate for these inconsistencies by curing a restoration multiple times from different locations, a cost-benefit analysis would show that the additional time required to cover and completely cure large restorations may not be worth the cost savings of purchasing a budget LCU.
Lack of accountability
The lack of serial numbers in some of the budget LCUs, the inconsistencies in manufacturing, such as the same brand of light (Woodpecker LED F) containing two different types of LED light sources, and the large coefficient of variation in the power outputs of most of the budget LCUs also speaks to the lack of accountability from some budget LCU manufacturers. Should a problem arise with a patient after using some of these LCUs, it would be impossible to contact the manufacturer because there was no contact information provided with the LCU.
Of note, although the Woodpecker lights are listed on the FDA site as having received 510(k) approval, the same could not be said for the Woodpecker style LED B Lights F and G that appeared to be copies of the Woodpecker LED B lights. They also had the same serial numbers, making it impossible to identify the individual LCUs (table 1).
Conclusions
Within the limitations of the study that measured the mean radiant power, coefficient of variation in the power values, the mean irradiance, and beam profiles from two examples of eight brands of budget LCUs and one LCU from a major dental manufacturer, it was concluded that:
1. The Paradigm DeepCure LCU from 3M, although the most expensive, delivered a high power (839 + 8.1 mW) that remained stable over 500 discharge cycles, had a uniform beam profile, the widest internal light tip diameter (9.2 mm), and had a low-profile light guide.
2. In contrast, none of the budget lights performed well in all categories. For most budget LCUs, the power output decreased with use.
3. Different examples of each brand of LCU behaved differently. Therefore, future studies comparing brands of LCUs should use at least two examples of each LCU.
4. Buyer beware when purchasing medical devices online. What appears to be a bargain may not be approved for use by the FDA on your patients.
Authors’ note: The authors wish to thank Stella Braga, Braden Sullivan, and Daniel Labrie for their technical assistance. In addition, Alia Osseiran was supported by a traveling scholarship provided by 3M Oral Care.
References
1. Worthington HV, Khangura S, Seal K, et al. Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst Rev. 2021;8:CD005620.
2. Nedeljkovic I, De Munck J, Vanloy A, et al. Secondary caries: prevalence, characteristics, and approach. Clin Oral Investig. 2020;24(2):683-691.
3. Price RB, Derand T, Sedarous M, Andreou P, Loney RW. Effect of distance on the power density from two light guides. J Esthet Dent. 2000;12(6):320-327.
4. Kojic DD, El-Mowafy O, Falenchuk O, et al. Radiant-exposure attenuation through class-2 proximal slots. Am J Dent. 2021;34(2):116-119.
5. Konerding KL, Heyder M, Kranz S, et al. Study of energy transfer by different light curing units into a class III restoration as a function of tilt angle and distance, using a MARC Patient Simulator (PS). Dent Mater. 2016;32(5):676-686.
6. Durner J, Obermaier J, Draenert M, Ilie N. Correlation of the degree of conversion with the amount of elutable substances in nano-hybrid dental composites. Dent Mater. 2012;28(11):1146-1153.
7. Fujioka-Kobayashi M, Miron RJ, Lussi A, et al. Effect of the degree of conversion of resin-based composites on cytotoxicity, cell attachment, and gene expression. Dent Mater. 2019;35(8):1173-1193.
8. Maktabi H, Ibrahim M, Alkhubaizi Q, et al. Underperforming light curing procedures trigger detrimental irradiance-dependent biofilm response on incrementally placed dental composites. J Dent. 2019;88:103110.
9. Price RB, Ferracane JL, Hickel R, Sullivan B. The light-curing unit: An essential piece of dental equipment. Int Dent J. 2020;70(6):407-417.
10. Bonsor SJ, Palin WM. ‘Let there be light,’ and there was light, but was it enough? A review of modern dental light curing. Dent Update. 2021;48(8):633-640.
11. Burke FJT, Mackenzie L, Sands P, Shortall ACC. Ten tips for avoiding post-operative sensitivity with posterior composite restorations. Dent Update. 2021;48(10):823-832.
12. Moreira RJ, de Deus RA, Ribeiro MTH, et al. Effect of light-curing unit design and mouth opening on the polymerization of bulk-fill resin-based composite restorations in molars. J Adhes Dent. 2021;23(2):121-131.
13. Harun NA, Santini A, Roebuck EM. The effect of interincisal opening, cavity location and operator experience on the energy delivered by a light-curing unit to a simulated dental restoration. Prim Dent J. 2014;3(2):26-31.
14. Andre CB, Nima G, Sebold M, Giannini M, Price RB. Stability of the light output, oral cavity tip accessibility in posterior region and emission spectrum of light-curing units. Oper Dent. 2018;43(4):398-407.
15. AlShaafi MM, Harlow JE, Price HL, et al. Emission characteristics and effect of battery drain in "budget" curing lights. Oper Dent. 2016;41(4):397-408.
16. Cardoso IO, Machado AC, Teixeira D, et al. Influence of different cordless light-emitting-diode units and battery levels on chemical, mechanical, and physical properties of composite resin. Oper Dent. 2020;45(4):377-386.
17. Shimokawa CA, Turbino ML, Harlow JE, Price HL, Price RB. Light output from six battery operated dental curing lights. Mater Sci Eng C Mater Biol Appl. 2016;69:1036-1042.
18. Drucker S, Gregg SM. Online purchasing: How to avoid “gray-market” dental products. Compendium. 2019;40(8).
19. U.S. Government Silver Spring, MD, USA. Code of Federal Regulations, Title 21--Food And Drugs Chapter I—Food and Drug Administration Department of Health and Human Services Subchapter H - Medical Devices Part 872 Dental Devices. 2020. Accessed April 1, 2020 Volume 8. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=872&showFR=1
20. U.S. Food and Drug Administration Silver Spring, MD, USA. FDA Premarket Notification 510(k). 2020. Accessed August 5, 2021. https://www.fda.gov/medical-devices/premarket-submissions/premarket-notification-510k
21. U.S. Food and Drug Administration Silver Spring, MD, USA. Guidance for Industry and FDA Staff Dental Curing Lights - Premarket Notification [510(k)] Submissions. 2006. Accessed August 5, 2021. https://www.fda.gov/media/74206/download
22. U.S. Food and Drug Administration. Example of a warning letter sent by the FDA to Andy Jassy, CEO Amazon.com, Inc. 2021. Accessed September 25, 2021. https://www.fda.gov/media/151096/download
23. Amazon Services Business Solutions Agreement. 2021. Accessed September 13, 2021. https://sellercentral.amazon.com/gp/help/external/G1791?language=en_US
24. U.S. Food and Drug Administration Silver Spring, MD, USA. Learn if a medical device has been cleared by FDA for marketing. 2017. Accessed August 5, 2021. https://www.fda.gov/medical-devices/consumers-medical-devices/learn-if-medical-device-has-been-cleared-fda-marketing
25. U.S. Food and Drug Administration Silver Spring, MD, USA. FDA Device Approvals, Denials and Clearances. 2018. Accessed August 5, 2021. https://www.fda.gov/medical-devices/products-and-medical-procedures/device-approvals-denials-and-clearances
26. ISO 10650 Standard dentistry-powered polymerization activators. International Standards Organization, Geneva, Switzerland; 2018. p. 15.
27. Harlow JE, Sullivan B, Shortall AC, Labrie D, Price RB. Characterizing the output settings of dental curing lights. J Dent. 2016;44:20-26.
28. Shimokawa CAK, Turbino ML, Giannini M, Braga RR, Price RB. Effect of light curing units on the polymerization of bulk fill resin-based composites. Dent Mater. 2018;34(8):1211-1221.
29. Soares CJ, Braga S, Price RB. Relationship between the cost of 12 light-curing units and their radiant power, emission spectrum, radiant exitance, and beam profile. Oper Dent. 2021;46(3):283-292.
30. Soares CJ, Rodrigues MP, Oliveira LRS, et al. An evaluation of the light output from 22 contemporary light curing units. Braz Dent J. 2017;28(3):362-371.
31. Shortall AC, Hadis MA, Palin WM. On the inaccuracies of dental radiometers. PLoS One. 2021;16(1):e0245830.
32. Shimokawa CA, Harlow JE, Turbino ML, Price RB. Ability of four dental radiometers to measure the light output from nine curing lights. J Dent. 2016;54:48-55.
33. Price RB, McLeod ME, Felix CM. Quantifying light energy delivered to a class I restoration. J Can Dent Assoc. 2010;76(2):a23.
34. Gallagher C, Gallagher V, Whelton H, Cronin M. The normal range of mouth opening in an Irish population. J Oral Rehabil. 2004;31(2):110-116.
Alia Osseiran, MPH, MS, is a dental student at TUSDM and expects to graduate in 2022. She earned her MPH concentrating in epidemiology from Boston University and her MS in biomedical sciences from Mississippi College. Ms. Osseiran is an active member of the American Dental Association and the Massachusetts Dental Society and serves on the board for the American Student Dental Association and the Joint Commission on National Dental Examinations. She can be reached at [email protected].
Richard B. Price, DDS, MS, PhD, is a prosthodontist and the director of digital dentistry at Dalhousie University, Halifax, Canada. He is actively involved in research on dental resins, curing lights, and teaching light curing. He has made numerous presentations, authored more than 190 peer-reviewed articles, and coauthored the chapter on light curing in the 7th edition of Sturdevant’s textbook Art and Science of Operative Dentistry. He can be reached at [email protected].
Katie Dunn, MAT, is the assistant director of predoctoral research at TUSDM in Dental Research Administration.
Duong Tran, DDS, MPH, PhD, is an assistant professor in public health at TUSDM.
Cristiane Maucoski, BDS, MS, is an orthodontist and currently a PhD visiting student researcher in the faculty of dentistry at Dalhousie University, Canada.
Gerard Kugel, DMD, MS, PhD, is the associate dean for research and professor of comprehensive care at TUSDM.
Editor's note: This article appeared in the February 2022 print edition of Dental Economics. Dentists in North America are eligible for a complimentary print subscription. Sign up here.