Digital radiography growing in popularity
By Paul Feuerstein, DMD
The busiest booths at recent dental meetings have been the digital radiography - otherwise known as DR - exhibits. Many doctors and staff appear to be hovering around computer screens with puzzled looks on their faces while smiling salespeople try to answer questions and give presentations during their shows. Courses on DR are sold out.
Nevertheless, many practitioners have not installed computers throughout their offices and are comfortable with traditional film. After speaking with a number of industry experts, I can say that for now, film is alive, well, and improving. Although there are a few film manufacturers, Kodak is still considered the market leader. A Kodak spokesman said there has been growth in both the film and digital sides of the marketplace. Kodak continues to improve film quality and density while decreasing the amount of radiation necessary to expose the film.
The new InSight Film has been a major advancement in both areas. This film, a silver halide (speed F), reduces radiation exposure up to 20 percent compared with Kodak Ektaspeed Plus Intraoral Dental Film (up to 60 percent compared with D-speed films). Incorporating patented Kodak T-Grain emulsion technology for excellent image quality and resolution without sacrificing speed, Kodak InSight Intraoral Dental Film also accommodates a wider range of processing conditions and is exceptionally tolerant of process variations. Factors such as the age of chemistry are less likely to impact image quality. As a result, dentists can choose a faster film speed to reduce radiation exposures - without requiring significant reengineering of processing practices. Kodak also has looked at the comfort issue and introduced Suresoft packets for better patient acceptance. Patients can be more at ease thanks to the soft, round, cushioned edge that covers the perimeter of the film packet.
Since nearly 80 percent of offices use film, we should examine the pros and cons. An existing office has already made the investment in processing equipment and in many cases, a dark room. Many offices use daylight loaders, eliminating this floor space. There are some interesting points in a recent article by Drs. Allan and Taeko Farman of the University of Louisville that discusses the pros and cons of film and the status of today’s digital sensors. There are ongoing costs of film, chemistry, mounts, disposal, and, of course, time. The latter is not only relevant in the processing and mounting time, but also in maintenance of the processors. This includes periodic cleaning of the machinery as well as common repairs of these units with several moving parts. Of course, some offices have been using the same processor for 20 years, and others may be doing all of this by hand in dip tanks. The problem with the manual system is an inconsistency of time and temperature as well as an inherent inefficiency of changing chemistry at proper intervals. This can lead to inaccurate results in the developed film. Kodak states that InSight is more forgiving but the office still has to take responsibility for proper maintenance. Kodak reports that less-than-optimum imaging will occur if processing conditions drift out of the ideal range. Processing chemistries must be replenished daily, mixed correctly, and stored at a temperature of 65 to 72 degrees (18.5 to 22 degrees C). Chemical cross-contamination also can make film appear foggy and dark. If the safelight lens (filter) is scratched, cracked, or damaged, it may leak enough light to fog the film.
Of course, if all of the rules are followed, film is an excellent diagnostic tool and is still the standard against which we compare the newer technologies.
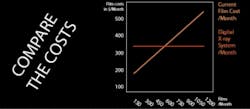
So what does film actually cost? Raw film is about 25 cents, but the real cost per film is about $1.18. Therefore, an office that takes 50 films per day will spend more than $32,000 in a three-year period. In a study done at UCLA and UCSF, authors Drs. Gratt and Sickles broke down the costs of taking and developing intraoral radiographs with both manual (dipping tank) and automatic processing systems. Looking at initial setup costs, one factor is the physical place in which the developing takes place. In manual and some automatic systems, a darkroom is necessary, and some plumbing expenses must be considered. This will yield an ongoing expense related to the space needed. The room can be as small as 3 feet by 4 feet, but with walls and such, it takes away otherwise usable space, even if only for storage or perhaps room enough for a panoramic radiography unit. The automatic processor has an initial cost, as well as associated maintenance. An automatic processor with a daylight loader only requires some counter space. There also are utility costs associated with running water (some older units have requirements for constant running water) and electricity to heat the solutions.
In terms of labor costs, there are three major factors: the actual taking of the images (which is a constant for all systems), processing the images, and mounting them in a suitable format and organizing them in patient charts. A review of several automatic processors shows the time to produce a dry archival film is four to seven minutes, averaging about five minutes. There is also daily, weekly, and monthly maintenance of the processor (or tanks), including time to replenish or refill solutions and clean the equipment. There are labor and material costs associated with these processes. We must also consider the disposal costs of solutions in this environmentally aware age. A labor cost associated with digital radiography is training time. In some offices, staff members must be familiar with computer use and programs as well as the physical change in taking radiographs.
When considering the apparent costs of digital radiography, the expenditure is already ongoing in the office budget. In addition, there are no extra costs associated with an increase in the number of images taken - the expenses (except for barriers at about 5 cents each) are constant. Assuming a total conversion to digital, the costs are actually less over time.
Many offices are still happy to continue using traditional film. They already have their X-ray heads which some have been using for more than 20 years. Those old, steel units weigh more than 100 pounds, require multiple 4-by-4s in the wall for support, and still are going strong. Some cannot cut the time fast enough to be used for the new digital sensors, thus adding an additional obstacle to the conversion. Many new DR users come from a hardware failure of this old equipment. As stated, the X-ray heads might go bad, and I don’t think you can easily find new circuit boards for a 1960s SS White controller. Or, the old Philips X-ray processor finally bites the dust. These sorts of crises occasionally drive doctors to think that if they must make an investment, it might as well be digital. After all, a tax credit is waiting. The problem to the shortsighted practitioner, though, is that the office first needs to establish a computer infrastructure plan. There is still an offering from the DR manufacturers that can stall that event. A couple of systems are sold with laptop computers that are self-contained and can be moved from room to room. With wireless connectivity, this can offload the images and data to a central or front-desk computer (if there is only one in the office) or even remain on the laptop indefinitely. Other companies sell a sensor attached to a portable tablet-type computer that is even easier to move. Although these solutions are good, it still will be necessary to incorporate the radiographs into some sort of centralized system.
Another in-between solution involves using scanners. These units, which need a transparency adapter, allow the office to use traditional film and make a digital copy. In order to copy full series in their mounts, panoramic, or cephs, the transparency top must be “full bed” - at least 8-by-11. Some less costly scanners have a small 2- or 4-inch light in the cover, which technically could be used to scan a few intraoral radiographs at a time, but this becomes impractical. Many of the practice-management software programs can read, store, and manipulate these scans as long as they are “TWAIN” compliant. This is a specification that must be explored by both the PM software and scanner companies. There are also some excellent stand-alone radiograph scanning products that can be purchased and used independently of PM software. Once scanned, the images can be manipulated as well as printed, emailed, and uploaded. One area in which film fails is duplication. Unless the office is using “double pack” film, a copy is tedious to make and certainly inferior to the original. Every practitioner has had the frustration of reading radiograph copies from another dentist and trying to get a decent diagnosis. Scanners (as well as copies of digital images) can help solve this dilemma.
A low-tech solution - but one that works - is using an intraoral camera or digital camera to photograph the radiographs and saving them as image files. Again, these can then be manipulated in the same manner as the scanned images.
In the next installment, we will examine the implementation of various digital systems and give the practitioner a roadmap for this installation.
Dr. Paul Feuerstein installed one of dentistry’s first computers in 1978. For more than 20 years, he has taught technology courses. He is a mainstay at technology sessions, including annual appearances at the Yankee Dental Congress, and he is an ADA Seminar series speaker. A general practitioner in North Billerica, Mass., since 1973, Dr. Feuerstein maintains a Web site (www.computersindentistry.com) and can be reached by email at [email protected].