CBCT and implants: Improving patient care, one implant at a time, Part 2
By Edward J. Mills, DDS
For more on this topic, go to www.dentaleconomics.com and search using the following key words: CBCT, implant dentistry, 3-D dentistry, practice benefits, Edward J. Mills, DDS.
In Part 1, Dr. Mills discussed the growing demand for implants among baby boomers and new generations of patients familiar with their choices of treatment options, detailed how 3-D imaging has emerged as the new paradigm for implantology, and provided comparative diagnostic applications of CBCT versus other tools.
Practice benefits: an essential treatment tool
In my practice, the team conducts a 3-D exam for every implant placement, major restoration case involving possible endodontic treatment on multirooted teeth, trauma cases consisting of a possible fracture, and anytime they feel that a 3-D evaluation of anatomical features might enhance the course and predictability of treatment outcomes.
Within a few minutes of a CBCT scan, a doctor is able to explore a 3-D image of the patient within implant planning software. The surgeon can zoom in or out on an image as well as rotate and scan it, taking mouth and tooth measurements to determine if implants can be placed and how many the patient requires.
Significant anatomic structures, nerves, and blood vessels can be traced and highlighted for easy recognition. These views enable the dentist to develop a treatment plan that includes ideal placement, most appropriate implant form, diameter and length of the implant, as well as esthetic considerations such as bite.
A doctor can then share the treatment plan with the patient. By including patients immediately in the analysis and treatment planning, they are more confident in the practitioner and more likely to accept the recommended treatment. In my practice, I’ve found that treatment acceptance is up to 90% when the patient is shown CBCT images. This increases the quality of patient care.
It is easy for treatment plans derived from CBCT scans to be sent to the referring doctor, a dental laboratory, or other dental practitioners on a CD, DVD, or USB drive. With such easily transportable 3-D images and software, patient evaluation and treatment planning can take place when clinicians are together or in separate offices.
Often complex treatment plans involve contributions from several clinicians viewing the same data from different educational backgrounds as well as clinical perspectives. The final treatment plan becomes an orchestration of well-sequenced treatment procedures such that the final clinical outcome is consistent with the patient’s expectations.
Sharing 3-D clinical information with specialists such as oral surgeons and plastic surgeons allows the clinical team to discuss clinical scenarios with an exceptional level of specificity. Today, 3-D imaging not only allows the making of surgical and prosthetic guides for dental and other medical applications, but it also assists other clinicians such as plastic surgeons, ENTs, and orthodontists. The result is greater perceived value by a wider network of patient care providers, exponentially enhancing the dental practice’s referral base.
As CBCT and its associated software become the industry standard, it will drive agility across the field. One reason is that 3-D imaging systems offer a significantly lower cost than medical CT scanners.
For example, the Kodak 9000 3-D system and Kodak 9000C 3-D system are now very affordable, even for general practitioners. The software that supports these systems condenses training time and aids communication between oral surgeons and referring doctors.
The Kodak 3-D imaging module quickly reformats DICOM files in such a way that valuable information can be shared with numerous treating clinicians, even if each practitioner does not own the diagnostic software. The Kodak 3-D imaging module can be distributed to all practitioners involved for free, along with the reformatted information or scans.
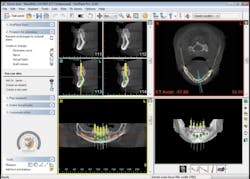
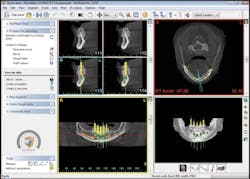
If a clinician prefers to analyze a patient's 3-D image with another software program — such as Simplant, NobelGuide, Keystone, Anatomage, or others — the original DICOM files are sent with the reformatted study. (See Fig. 1)
With its many applications and usability factors, CBCT is an essential tool not only for preimplant diagnosis and treatment planning, but also for guiding the procedure itself and evaluating the success of the implant (Dreiseidler et al.).
When sent to a lab, a surgical guide stent can be fabricated to ensure highly accurate placement. This yields a more predictable outcome, minimizes the chance of error, and ensures that all involved in a patient’s care are working from the same baseline data.
The greatest predictability on prognosis of implant survival is the quality of bone in which the implant is placed. The ability to accurately place implants of known lengths allows clinicians to safely insert implants closer to the alveolar nerve as compared to using 2-D images for this purpose.
With 3-D technology, it is simple to evaluate relative bone density between different sites, as well as the bone density in a cross-sectional manner. The ability to do so not only serves in establishing relative predictability of the treatment plan, but also may guide the clinician during surgery. The relative difference in the feel of low bone density compared to high-density areas acts as a tactile mapping during surgery. (See Fig. 2)
During the procedure, computer-aided implant plans can be applied as drill guides or navigation systems. The distance between implants and natural teeth is ideally 1½ mm, and between implants is ideally 3 mm, so that interproximal base is maintained and soft tissue contours are predictably reestablished.
Relative depth of implants to adjacent teeth has also been well documented. With CBCT imagery, practitioners are able to select the best implant and place it in such a way as to achieve optimal cosmetic results, as well as achieve the greatest predictability in exceeding patient expectations.
Immediate assessment and evaluation of clinical information allows the practitioner to modify and enhance treatment procedures on the fly, based on highly accurate information.
For example, this is particularly useful when using implants in immediate extraction sites. The natural assumption is to follow the trajectory of the root, as the implant needs to be placed lingual to the area of the natural root; the trajectory also needs to be lingual to the incisal edge of the adjacent teeth. When one places an implant via 2-D images, it can be difficult to identify a mesial or facial perforation without a buccal/lingual dissection.
Comparatively, 3-D imaging can more accurately convey the healing status of the implant. For example, one-week and one-year post-surgery 3-D models can be superimposed so that surface distances can be analyzed, which delivers a more complete visualization of the status of the implant (Abboud). (See Fig. 3)
Return on investment
Initially, most clinicians base their technology return on investment on the number of implants placed per week or month; however, I see a trend for dental professionals investing in 3-D technology in order to realize the full potential of the technology itself — not necessarily to increase the number of procedures conducted, but rather to enhance their authoritative position in the community, and to provide clinical data that enhances predictability and longevity of most restorative procedures.
Return on investment is not as clear-cut as a mathematical equation. If a practice does not own a 3-D scanner, it can only refer patients to other facilities for 3-D exams for initial assessments (Friedland). Also, the practitioner cannot easily obtain a scan postsurgically or restoratively.
For example, my practice charges for the initial scan, then conducts postoperative scans at no charge. Today’s patients are savvy consumers and know the value of certain medical procedures.
If patients obtain a CT scan in a hospital, they know it will cost between $1,000 and $1,500. If they can receive multiple CBCT scans in the office for only $395, patients perceive this as a bargain. Patients in turn perceive the scans as significant value-added services, which enhances their perception of the overall treatment value the practice renders.
In addition, the panoramic capabilities of hybrid systems, such as the Kodak 3-D extraoral imaging system, provide an additional source of revenue, which ensures a faster return on investment for dental and dental specialty practices.
Patient benefits
Dental implants are a safe, effective, low-maintenance solution for patients, particularly vis-à-vis prosthetics (bridges). Implants provide several practical, dental, and esthetic benefits.
Because implants last longer than bridgework and have a predictable and high success rate, they offer a long-term solution and cost savings. There is no need for additional surgery following the implant procedure, and patients will never need to deal with misplaced prosthetics or messy adhesives.
Dental implants do not require support from neighboring teeth, which offers tooth saving compared to traditional bridgework. While a prosthetic relies on adjacent teeth, affecting their quality, implants leave the patient’s teeth untouched.
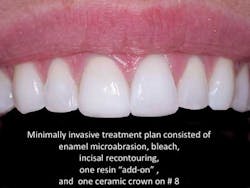
There is no bone creep. Lastly, because implants look and feel like the patient’s own teeth and integrate into the bone structure, they prevent bone loss and gum recession that often accompanies prosthetic devices. This not only provides a long-term, overall oral health benefit, it ensures there is a positive esthetic impact for the patient. (See Fig. 4)
Conclusion
Dental professionals are taking advantage of CBCT for diagnosis and treatment planning, as well as follow-up to implant procedures. CBCT has shifted the paradigm in implantology, from the identification of implant regions of interest and the associated maxillofacial structures, to the development and simulation of a treatment plan that includes ideal placement, most appropriate implant form, diameter and length of the implant, and esthetic considerations such as bite.
Using CBCT reduces the margin of error and minimizes radiation exposure to the patient, all while allowing the doctor to increase speed of treatment and streamline information sharing throughout the implant process.
For a practice to be able to obtain accurate imaging data that can be easily integrated within their practice management software also has multiple benefits. The ability to go to one source for solutions is incredibly valuable (i.e., time savings, no finger-pointing, etc.), especially if the source has a proven track record and focus dedicated to this technology.
One of the primary benefits includes the ability to evaluate and manipulate 3-D images anywhere in the practice, as well as off site. Also, the ability to easily organize imaging data by patient and make it accessible to multiple parties is critically important in our increasingly digital world.
If a dental practitioner considers an investment in 3-D technology, I recommend evaluating multiple systems — including visiting different offices using the systems — to determine which hardware and software programs make sense to their practice in particular. Understand that investing in 3-D technology is not necessarily about how it will fit into the practice today, but how it will shape the dynamics of the practice during the next two years and beyond.
References available upon request.
Edward Mills, DDS, is the founder of the Atlanta Center for Restorative Dentistry in Atlanta. A 1980 graduate of Emory University, he has lectured extensively throughout the world on state-of-the-art, restorative dental techniques. Dr. Mills is a fellow and past president of the American Academy of Implant Dentistry as well as a diplomat at the Board of Oral Implantology.