Ask Dr. Christensen
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics® readers. If you would like to submit a question
to Dr. Christensen, please send an e–mail to [email protected].
For more on this topic, go to www.dentaleconomics.com and search using the following key words: inlays, onlays, resin–based composite, indirect restoration, Gordon Christensen.
Q I have noticed a tendency among my colleagues who are involved heavily with promoting tooth–colored restorations to resist restoring intracoronal two– or three–surface carious lesions with resin–based composite. They are encouraging patients to accept indirect tooth–colored restorations, either milled in–office or made indirectly in a laboratory. I am encouraging patients to have tooth–colored restorations, but the majority of my smaller restorations are directly placed resin–based composite. Has there been a change in the thinking of the profession concerning when to place direct vs. indirect restorations in relatively small restorative preparations? Are indirect tooth–colored restorations better or worse than directly placed restorations in these small clinical situations? I am confused concerning what I should be doing.A Your question has at least two major ramifications — 1) financial feasibility and 2) the physical properties of the materials. Both are important. I will discuss the question from both aspects, and make suggestions relative to when direct and indirect restorations should be used.You know as well as I do that well–accomplished cast gold alloy restorations have long been the highest level of restorative service from a longevity standpoint for inlays, onlays, and crowns. However, the esthetic restorative emphasis for the last 30 years has made these restorations less desirable to patients. As a result, they are used by only a small percentage of practitioners.
Until relatively recently, tooth–colored indirect restorations have had a tumultuous history, evolving through several generations of less–than–acceptable restorative materials and cements, and causing dentists and patients significant frustration and financial loss.
As the professional and lay emphasis toward more esthetic restorations has matured, manufacturers have improved their restorative materials, bonding agents, and cements. Currently, laboratories make indirect restorations such as IPS Empress and IPS e.max. In addition, several tooth–colored, in–office milled materials from CEREC® or E4D Dentist® are serving well as onlays and inlays.
Does the success of tooth–colored indirect restorations mean that directly placed, resin–based composite restorations should be abandoned, and indirect laboratory made or in–office milled restorations should dominate restorative dentistry?
My response is a strong no! The reasons for my opinion and suggestions concerning how to use both indirect and direct restorations to take advantage of their best characteristics are as follow:
Financial considerations
Directly placed resin–based composite fees range from $146 for a one–surface posterior composite to $259 for a four–surface composite. The clinical time involvement to place a simple Class I or minimal Class II composite is only a few minutes in most restorative dental offices.
However, placement of a large MOD composite can easily require 30 to 45 minutes, and the procedure is relatively difficult. I don't think I have to convince you that using composite for all large MOD restorations would soon cause a dental practice to have severe financial difficulties. They are time– consuming and difficult to place and finish.
When considering the time and cost of indirect restorations, the financial picture and time needed for the procedures are very different from direct restorations. Statistics show that fees averaged $636 for a one–surface porcelain/ceramic inlay to $1,020 for a four–surface porcelain/ceramic onlay.
Of course, the laboratory cost for the indirect restorations — or the overhead cost for in–office milling devices — must be considered when comparing direct and indirect restorations. However, it becomes very clear that the indirect restorations are more financially acceptable than the direct restorations, especially when multiple restorations are made at the same time.
Restorative material physical characteristics
Historically speaking, fired, layered, feldspathic ceramic inlays and onlays have had mixed reviews relative to their clinical success. When placed well, they are acceptable, but many fracture during service.
However, the currently used ceramic and polymer tooth–colored restorative materials used for laboratory–made inlays and onlays have improved significantly in recent years. Some well–proven brands are IPS Empress, IPS e.max (which are ceramics), and belleGlass (which is a polymer). Millions of these restorations are in service, with far fewer fractures than with previous materials.
About 10% of U.S. dentists have in–office milling devices (CEREC or E4D Dentist). The ceramic and polymer materials used for milling have proven to be better than the materials used in dental laboratories for indirect restorations. Their physical properties are better than lab materials because the materials for milling are made into blocks in highly controlled conditions by the respective manufacturers.
Both in–vivo and in–vitro research projects have shown the acceptability of the restorations milled from these manufacturer–made ceramic or polymer blocks. Ceramic blocks are more popular by far than polymer blocks.
In other words, the materials currently used for tooth–colored inlays and onlays are very good. In my opinion, they won't compete with gold alloy, but they are reasonably acceptable and highly esthetic.
When should direct restorations be used?
Two factors are important when answering this question — time involvement and difficulty of placement. I have stated that large Class II resin–based composites require a significant period of time for proper placement, and noted they are difficult to place without problems. When is a restoration relatively simple, and when is a restoration difficult?
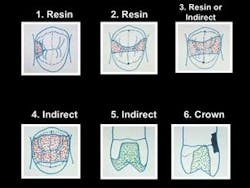
Fig. 1 shows my opinions on when direct and indirect restorations should be used.
Example 1 does not have any occlusal carious involvement. A simple direct composite restoration would require only a few minutes. The restoration would be financially acceptable, and the properly placed composite material would serve for many years. An indirect restoration would not be a good choice, since it would require removing significantly more tooth structure than the direct restoration. It would also cost the patient nearly four times more than the direct restoration.
Example 2 is similar to Example 1. When the isthmus width is one–quarter of the cusp–tip–to–cusp–tip distance — such as in the drawing — an indirect restoration is too aggressive and expensive, in my opinion.
Example 3 requires some thought. If the tooth has deep proximal box forms or if the patient is difficult to treat, an indirect restoration may be the better choice. If the box forms are shallow and the patient is cooperative, a direct restoration will probably be financially acceptable. Either direct or indirect restorative materials will serve adequately in this example where the isthmus width is only one–third of the cusp–tip–to–cusp–tip distance.
Example 4 leaves no choice from both a financial and material physical properties standpoint. A composite restoration for this preparation would require at least 30 minutes for most practitioners. The composite materials that would be used in this situation are questionable from a strength and wear standpoint. Of course, a competent practitioner could place composite in this situation, but it would not be the best choice.
Example 5 shows a tooth without any horizontal cracks or previous Class V restorations. The facial and lingual walls of the tooth are intact. An onlay covering one or more cusps is an appropriate choice. Third–party payers now accept coverage of one or more cusps as an onlay vs. an inlay, and many will pay for the service.
Example 6 shows a tooth with horizontal cracks in the remaining tooth structure, as well as a Class V restoration. Is there any choice for this restoration? Unless only a “patch” is planned, a crown is the most appropriate treatment from both a financial and physical standpoint.
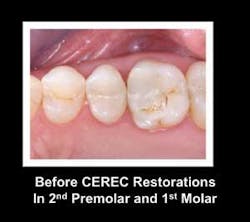
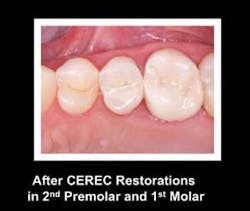
Fig. 2 shows two significantly broken–down teeth needing new restorations. These Class II restorations are large enough that significant time is required to restore them with direct resin, and the ability of the composite to support occlusal forces is questionable. They were restored with indirect ceramic restorations milled by a CEREC machine (Fig. 3, see page 70).
In summary, resin–based composite restorations placed well in conservative tooth preparations are feasible and acceptable financially, and the composite materials are very adequate for long–term service. There is no need to reduce the use of resin–based composite in the selected situations we have discussed (Fig. 4).
For those readers who would like to improve the speed of placement and the quality of their Class II resin restorations, please consider taking the “Esthetic Restorative Dentistry” course with me. Significant discounts are available for dentists up to five years out of dental school.
This hands–on AGD Mastership course includes faster and easier materials and techniques for composites, tooth–colored inlays, onlays, and crowns; veneers; bleaching, and how to best incorporate these procedures into your practice.
Call PCC at (800) 223–6569 or visit our Web site at www.pcc dental.com for more information.
Dr. Christensen is a practicing prosthodontist in Provo, Utah, and dean of the Scottsdale Center for Dentistry. He is the founder and director of Practical Clinical Courses, an international continuing–education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Rella) and senior consultant of CLINICIANS REPORT (formerly Clinical Research Associates), which since 1976 has conducted research in all areas of dentistry.