Implant placement vs. tooth retention
Q:
I've read various opinions on when to extract a tooth and place an implant. Assuming a patient has adequate financial ability to do either treatment, when should a tooth be extracted, and when should a tooth be retained, endodontic treatment accomplished, and a build-up and crown placed?
A:
In the past, when implants were not available, the decision was easier. However, now that placement of an implant in a healthy patient with adequate bone is relatively easy, the decision is more difficult. I will answer your question from several different angles.
Amount of coronal tooth structure remaining
Depending on the amount of coronal tooth structure remaining, a restored tooth has a different potential for long-term success. The following discussion of potential success is based on articles from the current conflicting evidence-based dental literature, as well as my own observations on the success or failure of thousands of endodontically treated, restored teeth.
1. Almost all of the coronal tooth structure remaining. Endo not necessary or endodontic access minimal-The potential for long-term clinical success with or without a crown on the tooth is excellent. Placement of an implant is not advisable.
2. Up to one-half of the coronal tooth structure gone. Endodontic treatment if necessary. Post and core placed or considered not necessary. Ferrule placed on areas where tooth structure missing. Nonabusive occlusion-If an adequate post and core is placed, followed by a crown or full occlusal coverage onlay, the possibility for long-term clinical success is excellent. Placement of an implant is not advisable.
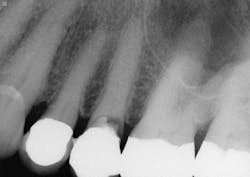
3. All supragingival coronal tooth structure gone. Endodontic treatment usually necessary. Post and core placed. Enough remaining tooth structure to allow at least 2 mm of ferrule around the margin portion of the tooth preparation, or bony crown lengthening accomplished allowing the ferrule. Nonabusive occlusion (Figures 1 and 2)-This clinical situation requires in-depth informed consent from the patient, since saving the tooth is expensive and the long-term success of the clinical result is questionable. If the treatment fails, an extraction, along with an implant and crown or a fixed prosthesis, will be required, further adding to the patient cost. The potential for success is markedly reduced in this situation. However, proper placement of a post and core and crown allows clinical success in a significant percentage of cases. If the patient feels more comfortable with an implant after proper informed consent, that treatment should be strongly considered. However, in my experience, many patients prefer to retain the affected tooth, in spite of the reduced potential for long-term service. That is also my personal preference.
4. All supragingival coronal tooth structure gone. Abusive occlusion. Endodontic treatment. Post and core placed. Enough remaining tooth structure to allow at least 2 mm of ferrule around the margin portion of the tooth, or bony crown lengthening accomplished allowing the ferrule-This clinical situation changes the success potential significantly. Presence of grinding or clenching bruxism can place forces on the affected tooth up to four or five times the forces of normal chewing. Based on the dental literature and my experience, I estimate that abusive occlusion is present in up to one-third of the adult patients in a typical general practice. The challenge with such patients is that implant placement also has a questionable long-term success potential because of the intense occlusal forces and the fact that implants do not move in the supporting bone while teeth do move significantly. If occlusion is not meticulously adjusted, the restored implant receives enormous forces on it, potentially breaking the crown on the implant or the opposing teeth. Also, occasionally the implant may not integrate. In such questionable cases, the patient should be informed fully about the chances for failure, and the treatment decision should be a mutual one between the dentist and patient. My personal preference is to retain the natural tooth if at all feasible.
5. All tooth structure gone to the bone. Endodontic treatment. Post and core placed. Not enough tooth structure to provide a ferrule. Nonabusive occlusion (Figures 3 and 4)-Orthodontic tooth extrusion is a technique seldom used in dentistry, but it can possibly save such teeth. In spite of being taught to dental students, I find in my CE courses that orthodontic tooth extrusion is seldom accomplished. If the tooth root is long, the technique can be successful. Additional cost to the patient is necessary, accompanied by the time for orthodontic tooth movement, and a period of bone stabilization before restoring the tooth. Crown lengthening is another option if such treatment will not cause an esthetic challenge. Presence of abusive occlusion adds a strong negative to this clinical situation. Most dentists do not accomplish orthodontic extrusion or bony crown lengthening. Therefore, removal of the tooth and placement of an implant remain as the most predictable and viable solution.
Cost for retaining a tooth or placing an implant
Assuming the patient has the financial resources to accomplish either procedure, the cost comparison using approximate ADA reported average fees is quite different as follows for a single root anterior tooth:
Cost to retain the tooth
• Endodontics ~ $700
• Post and core ~ $350
• Crown ~ $1,040
• Total ~ $2,090
Cost to remove the tooth and place an implant
• Extraction ~ $150 ~$150
• Place implant ~ $1,800 ~$1,800
• Screwed on crown ~ $1,400 or custom abutment ~ $775 & crown ~$1,040
• Totals ~ $3,350 ~$3,765
These fees assume that crown lengthening, periodontal treatment, or grafting were not necessary, which would change the numbers significantly. From a financial standpoint, retaining the tooth is significantly less expensive.
Patient desire to retain the natural tooth
Although the dentist is the authority and should make strong suggestions to the patient about the most adequate potential treatment, many patients request to retain the natural tooth. After placing implants for over 35 years, that is also my personal opinion, if it is possible.
Summary
It can be an easy or difficult decision to remove a tooth and place an implant. Patients should be involved in making that decision. Thorough informed consent should be provided, and a detailed discussion of the potential for success or failure should be made. The joint patient/dentist decision should be based on the amount of tooth structure remaining, occlusion, financial considerations, patient desire to keep the natural tooth, and patient acceptance of other needed procedures to retain the tooth. Either clinical procedure can be successful if all factors are considered and treatment is accomplished properly.
Gordon J. Christensen, DDS, MSD, PhD, is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Dr. Rella Christensen) and CEO of Clinicians Report (formerly Clinical Research Associates).