A candid appraisal of the state of the art for composites, adhesives, and cements in 2009
For more on this topic, go to www.dentaleconomics.com and search using the following key words: adhesives, resin–based composites, cements, Dr. Gordon Christensen, Focus On.
There has been a significant amount of confusion, contradiction, dogma, and lack of information about composites, adhesives, and cements. Practitioners have had to make their own decisions on numerous aspects of patient care because of the lack of agreement in the literature and advertisements on how to best treat patients with these products.
In an attempt to clarify answers to some of the confounded clinical questions, this article is based on my personal experiences of providing continuing education courses to tens of thousands of dentists for many years, asking innumerable questions of the continuing education attendees, visiting many clinical dental offices, dental schools, and research facilities, accomplishing my own in–vitro and in–vivo research, and answering thousands of questions annually asked by “real world dentists.”
My suggestions have also been influenced by the research presented in numerous international articles. However, often the in–vitro and in–vivo conclusions in the literature do not agree, and “human” decisions must be made about the topic. Are such personal decisions about the best way to accomplish clinical procedures justifiable? The following quotes will help answer that question and interpret the value of this article.
The author of “evidence–based medicine” (later espoused by dentistry), David Sackett, MD, a Canadian physician, stated, “Evidence–based medicine is the conscientious, explicit, and judicious use of currently best evidence in making decisions about the care of individual patients.
The practice of evidence–based medicine means integrating individual clinical experience with the best available clinical evidence from systematic studies.” In other words, both scientific studies and clinical observation must be combined. I completely agree! Sackett's statement is the basis of the following suggestions.
I will provide information relative to the state of the art for resin–based composites, adhesives for tooth structure, and dental cements. I will include my own observations relative to the use patterns of dentists, combined with the available research, and I will make suggestions for dentists, manufacturers, and retailers relative to apparent needed areas of change and improvement in the three areas.
Resin–based composites
During the 50 years since the introduction of these materials, there have been enormous improvements in all material characteristics. It would be difficult to identify a genuinely poor resin–based composite material currently popular on the market. Nearly all dental resin–based composites use the same resin chemicals, and similar fillers, initiators, and catalysts. With a few new and emerging exceptions, nearly all resins have similar polymerization shrinkage (about 2%).
Most resins cure with a light of the same wavelength. Nearly all resin–based composites can be finished and polished to a beautiful smooth finish with a multitude of good finishing and polishing products. In a recent comprehensive CLINICIANS REPORT clinical and laboratory study, Astropol/Astrobrush from Ivoclar Vivadent (Amherst, NY) and FlexiDisc/FlexiPoints/FlexiCups from Cosmedent (Chicago, IL) were the highest rated polishing products. All of the polishing materials and techniques used in the study produced smooth surfaces on various types of composites.
After observing the many similarities among resin–based composites, what is different among current composite brands? The only significant, clinically observable difference is retention of smoothness over a period of service. The following brief discussion helps to differentiate those products that remain smooth from those that become “frosty” in the mouth, thereby picking up food, beverage, and lipstick stains.
In my opinion, composite materials fit into just a few categories that differentiate them clinically. These categories are related to the type of filler content, which is further related to their ability to retain surface smoothness during service. However, there are many additional classifications of resins used by others for scientific purposes.
The majority of composites are “microhybrids.” The resin in these materials is filled primarily with relatively large glass particles (~400–600 nanometers in size) surrounded by small particles of usually silicon dioxide (~40 nanometers). These light curing materials are strong, resist wear well, and have good color stability. However, almost without exception, they develop a “frosty” appearance after a few months of service in the mouth. This characteristic is of no concern in areas that are not involved esthetically, but in large Class IIIs, Class IVs, and resin veneers, restorations made from these resins often become rough, stained, and disagreeable to discerning patients.
In the past few years, the 3M ESPE (St. Paul, MN) product Filtek Supreme Plus has dominated the North American market. Why? This “nanofill” material has physical strength characteristics similar to the described microhybrids, but it is filled with extremely small particles of zirconium oxide (under 100 nanometers in size) that have been sintered (fused) into larger agglomerates. The result of this clever physical process is a material that is strong and retains its smoothness. (Fig. 1)
The word nanofill infers that all of the particles are less than 100 nanometers. That means that they are many times smaller than the particles that are present in microhybrids, and explains the retention of relative smoothness over a service period.
The highly patented “nano” technology has stimulated other companies to produce what some are calling “nanohybrids.”
These products have glass particles similar in size to microhybrids, but most of them have been filled additionally with nano particles. They retain smoothness better than current microhybrids. Example products are Esthet–X HD from Dentsply Caulk (Milford, DE), Herculite Ultra from Kerr (Orange, CA), IPS Empress Direct from Ivoclar Vivadent (Amherst, NY), Kalore from GC America (Alsip, IL), and Renamel Nano from Cosmedent (Chicago, IL).
Only time, continued clinical usage, and critical observation will determine if these products retain their smoothness over a long period of service. In–vitro studies are stating that they do, but in my experience, in–vitro laboratory studies on this topic are seldom representative of actual smoothness retention in the mouth.
A relatively unknown product in the U.S., Estelite from Tokyama (Encinitas, CA), has been well received by practitioners for both its strength and smoothness, as observed over several years of service (~200 nanometers particle size).
The smoothest materials over long–term service in the mouth are still the microfills, introduced many years ago. These include Durafill from Heraeus Kulzer (Armonk, NY), Renamel Microfill from Cosmedent (Chicago, IL), and Heliomolar from Ivoclar Vivadent (Amherst, NY). All three products contain silicon dioxide fillers under 100 nanometers. However, it is well known these materials must be used in thin external layers over stronger internal microhybrids, nanohybrids, or nanofills, since microfills are not as strong as the previously described materials and can fracture in service if placed in layers greater than 1 mm to 1 ½ mm. (Fig. 2)
Summary of resin–based composites
Current composites are excellent if used with appropriate clinical procedures. Try to find a bad brand. Lower polymerization shrinkage products are on the market, such as Filtek LS from 3M ESPE (St. Paul, MN). They have yet to become popular in North America, but time will tell if dentists feel the clinical need for improvement in this characteristic.
Retention of surface smoothness over time is the only apparent major clinically significant difference among the current materials that has motivated dentists to change products, and that difference is important only in certain previously described clinical locations.
Adhesives
The evolution of products that bond to tooth structure has been an amazing but slow process over 50 years. Enamel bonding, now well–known and trusted by practitioners as a strong and long–term bond, has not changed significantly since its invention in the late 1950s.
The first category of products that created relatively adequate in–vitro bonds to dentin is now described as the fourth generation of bonding agents. It is typified by the 3M ESPE (St. Paul, MN) product, Scotchbond Multi–purpose, and this total–etch product it is still a very adequate material. It uses three components — acid etch, primer, and unfilled resin — and this “total–etch” product removes the “smear” layer in its entirety.
When used meticulously, the fourth generation, or what have been described as total–etch bonding agents, work very well. However, used improperly, they have been shown to produce postoperative tooth sensitivity and some pulpal death.
Dentin bonding has stimulated an unbelievable amount of academic research, but in spite of high in–vitro bond strengths, practitioners know dentin bonding to be an unpredictable bond, best augmented with mechanical retention for long–term clinical success.
In surveys I have conducted among practicing dentists, prevention of postoperative tooth sensitivity ranks much higher in their desired characteristics than bond to dentin.
Postoperative tooth sensitivity when using resin in Class I and II restorations was a major problem a few years ago, as reported by a survey of nearly 5,000 dentists.
But practitioners have learned how to prevent it by using so–called sixth and seventh generation self–etching bonding agents that do not remove the “smear layer,” or by using resin–modified glass ionomer liners such as Fuji Lining LC from GC America (Alsip, IL) or Vitrebond from 3M ESPE (St. Paul, MN) (Fig. 3), or by placing a self–etching primer followed by a flowable resin.
By far the most popular brand of bonding agent in recent years has been the self–etching Clearfil SE Bond from Kuraray (New York, NY). (Fig. 4) In–vitro research projects show this product to produce one of the highest bonds to dentin, but also show that lower bonds to enamel are produced by most self–etching brands, including SE Bond.
As a result of the research, many dentists use a small amount of standard phosphoric acid gel carefully placed on just the enamel margins and washed off very rapidly before doing the self–etch procedure. Some researchers are critical of this technique, claiming that the acid cannot be washed off without getting some of it on the dentin, thus reducing the dentin bond to be subsequently produced by the self–etch primer. In spite of the criticism, practitioners continue to use the procedure with success.
Most North American dental practitioners use self–etching bonding agents under resin–based composites instead of total–etch products. The use of self–etching products has been stimulated by the clearly proven major reduction in postoperative tooth sensitivity. This popularity reaffirms dentists' interest in lack of postoperative tooth sensitivity over higher reported in–vitro bond to tooth structure.
Summary of adhesive agents
Practitioners are tired of hearing about the purported superiority of one brand of bonding agent over another. Their main concern is to send patients home with restorations that are esthetically pleasing and predictably nonsensitive. These characteristics are mandatory when producing these low revenue restorations that are placed several times per day in typical practices. Self–etching bonding agents will continue to be popular because of their reduction or elimination of postoperative tooth sensitivity. Although in–vitro bond to dentin is readily obtainable and measurable, practitioners do not trust its long–term service, and bond to enamel is still the “gold standard” bond to tooth structure.
Cements
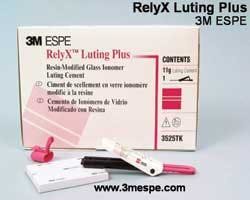
After several decades of watching cements come and go, practitioners are finally pleased with the current popular category, resin–modified glass ionomer, FujiCEM from GC America (Alsip, IL) and RelyX Luting Cement from 3M ESPE (St. Paul, MN). In my observation, this category is used by almost all North American dentists as their standard cement. These cements bond to tooth, expand and contract in a similar manner to tooth structure, release fluoride and recharge with fluoride, have adequate strength, are relatively insoluble, and most importantly, seldom produce postoperative tooth sensitivity.
What more do you want for routine cementation? These cements have been used in so many thousand clinical situations that it's doubtful we'll have another cement fiasco, as in the past. (Figs. 5 and 6)
Because of the need for additional strength and bond to tooth structure, some all–ceramic restorations, such as IPS Empress from Ivoclar Vivadent (Amherst, NY), are best used with resin cements such as Panavia F from Kuraray (New York, NY), or Multilink Automix from Ivoclar Vivadent (Amherst, NY). (Fig. 7)
In spite of the popularity of resin–based glass ionomer cements for routine cementation, the slight setting expansion of these cements has been shown to crack such restorations while in service, and resin cement is the proper choice.
The relatively new category of resin cement that contains self–etching primer is popular with some dentists because of minimal postoperative tooth sensitivity and moderate strength, including RelyX Unicem from 3M ESPE (St. Paul, MN), and Maxcem Elite from Kerr (Orange, CA).
Some in–vitro research shows minimal bond to dentin, but as with bonding agents, most dentists are more concerned with tooth desensitization than with bond. When fluoride prevention is not needed but strength is needed, such as in a bruxism or clenching patient, these cements have significant potential.
Summary of cements
Resin–modified glass ionomer is nearly ideal for routine cementation. Resin is indicated when more strength and bond to tooth structure is desired, and resin containing self–etching primer is indicated for some situations that require both moderate strength and minimal to no postoperative tooth sensitivity.
Summary
Bread–and–butter dentistry demands predictable and well–proven resin–based composites, adhesive agents, and cements. All of these products are used every day in typical dental practices. The state–of–the–art clinical success for each of these categories is highly acceptable if dentists and dental assistants use them properly. Popular, effective products and clinical techniques have been identified and discussed.
References available upon request.
Dr. Christensen is a practicing prosthodontist in Provo, Utah, and dean of the Scottsdale Center for Dentistry. He is the founder and director of Practical Clinical Courses, an international continuing–education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Rella) and senior consultant of CLINICIANS REPORT (formerly Clinical Research Associates), which since 1976 has conducted research in all areas of dentistry.