Ask Dr. Christensen
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics® readers. If you would like to submit a question to Dr. Christensen, please send an e-mail to [email protected].
For more on this topic, go to www.dentaleconomics.com and search using the following key words: soft tissue cutting, electrosurgery, diode laser, cutting procedures, implants, periodontal therapy, third-party payer, caries detection, radiographs.
by Gordon J. Christensen, DDS, MSD, PhD
Q I have read advertisements and articles promoting lasers in many dental magazines. The promoted advantages seem to be convincing. However, I have used electrosurgery for soft-tissue cutting with success for 20 years. Do the advantages of laser over electrosurgery for cutting soft tissue warrant purchase of an expensive laser?
A The question you asked has been argued for at least two decades, and the argument still rages. Cutting soft tissue with electrosurgery has been practiced for nearly 100 years. The concept was developed by Bovie at Harvard from 1914-1927. Electrosurgery techniques are well-known and successful. Although electrosurgery is not taught in some dental schools, most dentists have electrosurgery devices and they use them on a daily basis.On the other hand, the laser is a relatively new concept, used by approximately 10 percent of U.S. dentists. Laser use is growing in dentistry, and the diode laser is the most popular type.
The advantages of electrosurgery are well known (Figure 1). They are:
- Electrosurgery cutting is easy and fast.
- When adjusted properly, electrosurgery cutting is consistent and predictable.
- Electrosurgery electrodes may be bent to meet the surgical need.
- The electrodes cut on their sides as well as on the end.
- Hemostasis is produced relatively easily by electrosurgery.
- Electrosurgery cutting produces a near painless wound.
- With careful, gentle cutting, only slight trauma is produced.
- The electrode is self-disinfecting, but should still be sterilized.
- Electrosurgery devices are about 1/20 the cost of the least-expensive diode lasers. Usually, diode lasers are the least expensive of all dental laser types. Other types of lasers cost many times more than diode lasers.
The disadvantages of electrosurgery are:
- Patients must be anesthetized.
- The word electrosurgery causes fear for some patients. The word radiosurgery seems to be less objectionable.
- A burning flesh odor is produced when cutting.
- A burning flesh taste is present after cutting.
- The devices cut fast. As a result, there can be low tactile sense while cutting.
- The heat produced while cutting disallows monopolar electrosurgery use around implants. Most electrosurgery units are monopolar (bipolar electrosurgery devices can be used near implants).
The information that follows lists the advantages and disadvantages of the diode laser (see Figure 2). I suggest that you compare them with electrosurgery use.
- A minimal amount of local anesthetic or none at all is needed for laser use.
- The laser does not harm dental hard tissue.
- Judicious use of a laser should not injure the dental pulp.
- With care, a laser can be used around implants.
- There is growing evidence of the value of the laser for periodontal therapy.
- Laser use is antimicrobial.
- The laser removes endotoxins from root surfaces.
- Lasers are a significant marketing tool. Patients believe lasers to be state-of-the-art, and are excited by them.
The disadvantages of diode laser use are:
- The cost of a laser is far more than for electrosurgery.
- There is a learning period as practitioners become accustomed to use of a laser.
- Cutting soft tissue with a laser is slower than with electrosurgery.
- Care must be taken to avoid damage caused by the laser beam.
- Some laser techniques are time-consuming when compared to the use of a scalpel or electrosurgery.
- Other modes of treatment such as a scalpel or electrosurgery can accomplish many of the techniques considered to be laser techniques.
Are the above stated advantages of a diode laser more appealing to you than the advantages of whatever techniques you are now using to cut or remove oral soft tissues? The decision to use a laser instead of a scalpel or an electrosurgery unit is a personal one that you must make. The following information will summarize my personal feelings relative to making the decision to use a laser or electrosurgery.
Electrosurgery has been used for a long time and is well-proven as a soft-tissue cutting modality. It is relatively low cost, fast, easy, and predictable, but it produces some disagreeable odor and taste.
On the other hand, a diode laser is more expensive than electrosurgery, it is slower cutting than electrosurgery, but that may be an advantage for some clinicians. Diode laser cuts are less invasive than electrosurgery because of the slower cutting. Growing research is suggesting that a laser can be an acceptable treatment for periodontal disease, and it has tremendous patient appeal and acceptance. Both electrosurgery and the diode laser are viable treatment modalities.
Both electrosurgery and diode lasers are highly useful. Dentists have widely varied opinions on the subject. I use electrosurgery more than I do the laser.
Our newest video demonstrates soft-tissue cutting with both laser and electrosurgery on animal jaws, beef, and two patients. The video also shows the comparative use of diode laser and electrosurgery on pig jaws and beef, and it demonstrates laser and electrosurgery clinical techniques on human soft tissue.
Contact Practice Clinical Courses at (800) 223-6596 or visit www.pccdental.com for more information on V4324, "Cutting Soft Tissue, Laser or Electrosurgery."
Q Recently, a preauthorization treatment plan was turned down by one of my third-party payment programs on the basis that the carious lesions on the proximal surfaces were too small to restore. When should I cut a tooth for a restoration, and when should I not restore the tooth? What is the depth of carious lesion that warrants a restoration?
Using either analog or digital radiographs are the currently available methods for determining the presence of proximal caries. I have the following suggestions, which may or may not satisfy the requirements of your third-party payment company.
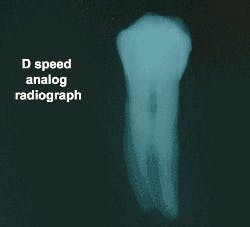
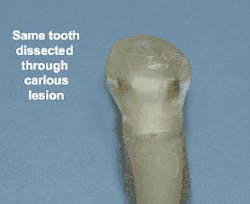
Figure 3 shows the D speed analog radiographic image of mesial and distal carious lesions in the tooth. Figure 4 shows the actual caries in the dissected tooth. It is obvious that the D speed analog film shows only a small portion of the full extent of the caries. Digital radiographs can be colored, textured, and expanded in size, as well as have the contrast changed. Even with these manipulations, initial caries eludes detection most of the time.
Research at CLINICIANS REPORT has indicated that the currently used bitewing radiographs, whether analog or digital, show only about one-half of the depth of the actual carious lesion. This percentage is a good guide for me when making clinical decisions. If the lesion is at least one-half of the way to the dentino-enamel junction, the odds of the lesion extending into the dentin are high. In a caries-active patient, I would restore such lesions. In a caries-inactive mouth, I would observe the lesion for at least one recall appointment to determine if it"s active before restoring it.
Your third-party payment program may disagree with me, but I look seriously at restoring carious lesions that have progressed one-half of the distance to the dentino-enamel junction, as viewed on any currently available radiograph. If the carious lesions show only minimally on the radiograph, it is a good idea to make a digital photo of the lesions when the teeth are partly prepared, providing photographic evidence that the lesions were present if questioned subsequently.
Dr. Christensen is a practicing prosthodontist in Provo, Utah, and Dean of the Scottsdale Center for Dentistry. He is the founder and director of Practical Clinical Courses. Call PCC at (800) 223-6569 or (801) 226-6569.