HOW TO PROFIT FROM... endo
Finding the fair fee for endodontics
Clifford J. Ruddle, DDS, FICD, FACD
A volcanic eruption best characterizes endodontic treatment in recent years. This massive, upward thrust of clinical activity largely can be attributed to general dentists and specialists who are better trained. This evolving story is dependent on consumers favoring canal treatment rather than extraction. This increase in endodontics is parabolic in that millions of teeth have been salvaged through combinations of endodontics, periodontics, and restorative dentistry. The purpose of this article is to illuminate certain "financial factors" of endodontic practice that influence quality, fun, and profitability.
The first financial factor is the comparison of interdisciplinary fees. Endodontic fees are the most undervalued of all dental services. The reasons behind this assertion are multi-faceted, complex, and historically-based.
Endodontics, for example, was the last specialty to be recognized(1963) by the American Dental Association (1963). In comparison, the ADA first recognized oral and maxillofacial surgery in 1947, orthodontics in 1950, pedodontics in 1948, periodontics in 1948, and prosthodontics in 1948. One significant milestone of specialty recognition is the formation of graduate programs that generate the science, basic research, training, and clinical procedures necessary to nurture, support, and secure a specialty`s future. Specialties perfect their clinical actions and generate predictable treatment outcomes. Naturally, fees are commensurate with the value their services provide and rise steadily over subsequent decades.
Regretfully, endodontic fees have not enjoyed this success story. Today`s endodontic fees generally are low and do not reflect the time, energy, effort, technological costs, and training needed to perform a service that is the very cornerstone of restorative and reconstructive dentistry. Much of our pre-1963 efforts were done without the benefit of science and basic research. As a result, the field of endodontics primarily experienced anecdotal results. Low endodontic fees reflected our self-esteem and the lack of belief that we could generate predictable outcomes. When endodontics worked, we were thrilled. If it failed, the profession`s attitude was nothing ventured, nothing gained.
In general, endodontic fees need to increase to reflect the time expended and be on par with fees assessed for the time spent performing other services. Getting a fair fee for the time spent would encourage dentists to reach their potential, aspire to greatness, and achieve predictable results.
1. Diagnosis is the pot of gold
At the end of the rainbow, there is said to be a proverbial pot of gold. Many practitioners are improving their annual income by performing more endodontic procedures, catapulting this discipline into an increasingly important profit center. However, the "real" endodontic pot of gold typically is not discovered.
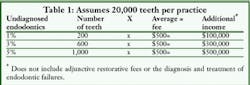
The second financial factor of this article is that, if diagnosed, endodontics could represent over $300,000 (see related article) of additional income per practice, not to mention the subsequent restorative procedures and related fees.
Interestingly, clinicians routinely are trained to perform a complete intraoral hard- and soft-tissue examination. Yet, how many dentists know the pulpal status of their patients` teeth? Unfortunately, most endodontic problems are diagnosed and treated according to subjective symptoms. The profession`s most revered test, percussion, and a radiograph often are the only information obtained to determine odontogenic health. A thorough endodontic examination is multifaceted and is comprised of vital pulp-testing, recording important physical findings, and obtaining two to three different, well-angulated, pre-operative radiographs.
If a complete endodontic examination were conducted on each patient, then a staggering and sobering number of quiescent, pulpally involved teeth would be identified, and could be ethically addressed before proceeding with other dental services. At the very least, an endodontic concern could be discussed with the patient, including the ramifications of no treatment. Or, those patients could be appointed for root-canal treatment or scheduled for future observations.
How big is the pot of gold? As a conservative example, assume a practitioner has 1,000 patients. Assume these patients have an average of 20 teeth each. Then, each dentist is the custodian of 20,000 teeth. Look at the endodontic possibility if pulpally involved teeth are not diagnosed between 1 to 5 percent of the time. Finally, assume if these teeth were diagnosed and treated, then the average endodontic fee would be $500 per tooth. My assertion is that the pot of gold is present, can be found, and its source is within the teeth that visit you daily.
2. Bridging the training gap
One important factor influencing endodontic profitability is training. Many dentists received their dental-school training years ago. The field of endodontics has grown exponentially in recent years, leaving many dentists in a gap between their previous training and current possibilities. Regretfully, an abundance of endodontic myths, misinformation, and misconceptions still are very much present. New and improved concepts, strategies, and techniques have simplified endodontic procedures, making them (in most cases) predictable and efficient.
The third financial factor is that excellent training gives a clinician the mindset and techniques to not only diagnose, better but to then perform procedures that are successful, safe, efficient, fun, and, yes, profitable.
Training is an investment in yourself. Doctors frequently ask me about how to select the right training program and instructor. An old saying is, "To see the teacher, look at the student."
Good training will critically impact performance. Training should not be an infrequent, spontaneous, or anecdotal act; rather, it should be a program that provides a carefully planned roadmap towards your practice vision. Training is an ongoing effort, is structured, and is periodically scheduled to keep you focused on the endless journey towards practice excellence. Training develops skills, passion, and joy during a performance, and it empowers the clinician towards greater achievement.
Performance in any endeavor is elevated by cross-training. Endodontic training can occur in a variety of formats, such as dental meetings, seminars, publications, videos, CDs, study clubs, or interactions with fellow colleagues. In my experience, the best training possible is in small interactive groups where the emphasis is on participation - i.e., hands-on courses. First-rate training is an investment that will improve results and increase income over time.
3. Finding technology that works
The emergence of new endodontic technologies, instruments, and materials has sparked new practice-building techniques. However, this accelerating rate of change also has left many dentists in a position of working harder, not smarter.
For many practitioners, the challenge is identifying which new technologies truly offer improvement in patient care, simplify procedures, and decrease chairtime compared to more traditional approaches. In addition, with change occurring at such a rapid rate, authentic concerns arise and linger: If we invest, train, and gain confidence in a technology, will it quickly become obsolete as a result of yet another emerging new technology?
The fourth financial factor is that innovative technologies exist, and they make endodontic treatment more predictable, faster, fun, and empowering to the dental team. Examples of certain beneficial new technologies that deserve a look include anesthetic delivery systems, computerized-digital radiography, microscopes, ultrasonic systems and instruments, electric handpieces, rotary nickle-titanium shaping instruments, heat-transfer units for thermosoftening gutta percha, and warm gutta-percha delivery systems.
Certain technologies have gotten the endorsement of international endodontists because, simply stated, they work. Clinicians need to be open to change and candidly discuss these new innovations with fellow colleagues they know and trust. With this information, clinicians can intelligently integrate the best technologies into their practices. Clinicians should consider a new product in terms of claimed advantages, safety, cost, and the potential for improved patient care. The right technologies can establish you and your practice as a center that is state-of-the-art and that delivers treatment excellence for its patients.
4. Disposable instruments
For almost 25 years of clinical practice, I have advocated that endodontic files be considered a disposable item, factoring their costs into the case fee. Specifically, I discard all hand and rotary nickel-titanium cleaning and shaping files following endodontic treatment on any given tooth, regardless of the number of canals, extent of calcification, degree of curvature, and canal length. If it isn`t practical, for whatever reason, to perform one-visit endodontics, then all instruments are saved, sterilized, and used to complete treatment during the next visit.
The cost of discarding all used files ranges between $20 to $40 per case and should be added to the endodontic fee. Clinicians need to be open-minded about the "disposable instrument" issue. Let`s look at the significant advantages of `single` instrument use.
- Safety. The episodes of broken instruments will be dramatically reduced and nearly eliminated when files are used correctly and discarded after single-tooth use. The risk of breakage increases sharply when hand or rotary shaping files are reused. The decision to throw out instruments after a single case is not just due to the degree of curvature or recurvature of a canal. More importantly, other variables influence the decision - the extent of calcification, the length of a canal, metallurgical factors, quality of manufacturing, and method of use.
When an instrument does break, think of the significant cost of attempting removal, possibly reappointing, patient discussions, record keeping, specialist consultation and at times referral, possible surgery or the loss of a tooth, patient confidence, and your peace of mind. It is especially wise to discard rotary instruments after a single use as they perform dramatically more work per unit of time compared to hand instrumentation.
- Efficiency. Studies have shown that all files lose approximately 50 percent of their cutting efficiency after very limited use. Starting every case with a set of new instruments equates to performing canal preparation with greater efficiency. In my training center, students prepared canals approximately five minutes quicker when using new vs. used instruments that previously had prepared no more than four canals.
There is a considerable improvement in profitability by using new files. Calculate the number of canals you treat per week and then per year; multiply this number by five (minutes) to identify the total number of minutes saved per year. Divide this number by 60 minutes to get the annual saved hours. Finally, multiply this number by your hourly target production to get the magnitude of dollars per year saved using new instruments. Despite the cost of single use, your decision to use new instruments for each case should be obvious.
- Instrument sterilization. Staff members` time is better utilized when they don`t have to collect and evaluate files for any obvious sign of metal fatigue, then put the instruments through the sterilization chain. Furthermore, safety is enhanced when the staff isn`t unnecessarily handling instruments.
- Patient perception. In today`s world of infectious diseases, strict protocols for sterilization, and patient concerns regarding these issues, starting each case with new instruments is a practice-builder and typically is appreciated by patients.
5. Just one visit
Scheduling rationales are as varied as the belief systems of practicing clinicians. Correctly scheduling patients for endodontic treatment has many advantages for patients and dentists alike. In the context of this article, one advantage of scheduling sufficient chairtime to properly and comfortably perform one-visit endodontics is to increase your annual income thousands of dollars per year.
In my specialty practice, emergency patients are seen promptly, and all other endodontic patients are routinely scheduled for a consultation appointment. Whether you see a patient on an emergency basis or for consultation, valuable information can be obtained that will guide your decision about how much time will be required to complete the treatment.
The invaluable consultations communicate all clinical and radiographic findings, anticipated challenges, prognosis, follow-up treatment, treatment alternatives, and, if appropriate, the chance to confer with other dental or medical professionals. The consultation appointment eliminates the stress of doctors thinking they are obligated to start a procedure and patients feeling pressured to begin treatment. More importantly, consultations allow your staff the opportunity to sequence future treatment and make financial arrangements.
In addition, consultations provide an opening for effective scheduling, the sixth financial factor.
Let`s look at a hypothetical case to determine the financial impact of scheduling. You are treating a molar, and the canals are cleaned and shaped. The master cones are fit and verified. All of the technical aspects of the case clearly are in your mind. At this point, you need perhaps 10 to 15 minutes to complete the case. But, due to other conflicts with time, you elect to reschedule the patient for treatment completion on another visit. How much does it cost you to reappoint this patient for another visit?
Five endodontists treating 15,000 patients identified a specific list of "events" and then recorded the average time spent duplicating these nonproductive, redundant events during a reappointment:
- Opening chitchat - 5 minutes
- Giving and obtaining anesthetic - 10 minutes
- Isolation, re-entry, refreshing canal(s), confirming apical file(s), cone adjustment, and confirmation - 10 minutes
- Temporize and post-op instructions - 3 minutes
- Closing chitchat - 2 minutes
The total amount of nonproductive reappointment time, then, is 30 minutes.
Obviously, these times can vary according to personalities, tooth position, number of canals, amount of interappointment time, etc. Regardless, the large pool of 15,000 patients reveals information that can be evaluated and used to more effectively schedule patients.
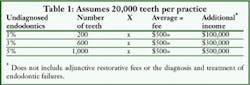
The annual lost income due to rescheduling is based on several variables, such as your target hourly production, how many endodontic procedures must be rescheduled per week, the amount of nonproductive time associated with each rescheduled visit which, if 30 minutes, costs you one-half of your target hourly production, and the number of weeks you practice in a calendar year. Each clinician can track, record, and analyze his/her specific numbers to fully reveal the cost of endodontic rescheduling (see table 2).
One-visit endodontics provides additional savings by eliminating the duplication of disposables that become necessary if a second visit is scheduled. Such scheduling also eliminates setting up and breaking down the operatory, repeating sterilization procedures, and the assistant`s time performing these tasks.
Of critical importance, one-visit endodontics allows a new productive procedure to be scheduled instead of rescheduling an uncompleted treatment. If this news isn`t bad enough, the patient you were minutes away from packing is not rescheduled for just 10 to 15 minutes, right? Clearly, one does not finish the case based solely on financial issues; rather, a case is finished when it has been treated to the best of one`s training and honest effort.
6. Endodontic fees
The seventh financial factor is endodontic fees for conventional treatment (clean, shape, pack) and nonsurgical retreatment. The chair- time and costs associated with any procedure need to be carefully analyzed and understood by the clinician, as well as communicated to the patient. Certainly, if one does not have the experience in endodontic treatment or retreatment, one may not be willing to invest the chairtime required to perform some of the tedious tasks necessary to achieve success. Obviously, the length of chairtime is going to affect the cost.
A fair fee is one that a patient pays with gratitude and a doctor receives with pleasure. Certainly, many treatment cases cannot be pigeon-holed or categorized according to insurance codes. What is a fair fee for properly diagnosed and well-performed treatment that has an excellent endodontic prognosis? My philosophy on conventional endodontic fees is best described by a formula used to compare procedural costs: The root-canal treatment fee plus the restorative-treatment fee equals the alternative-treatment fee.
Obviously, any endodontically involved tooth could be extracted and no further treatment performed. However, in the context of modern dentistry, the alternative treatment is typically, if possible, a bridge, a restored implant, or perhaps a partial denture. Since most patients prefer fixed dentistry, their alternative treatment cost to replace a missing tooth would equate to the fee assessed for a bridge or the fees for all procedures leading up to, and including, a restored implant.
For this hypothetical discussion, assume the endodontically treated tooth needs a post/core buildup and a crown. To further analyze the total fees associated with each treatment option, subtract out the lab cost on both sides of the equation.
Regardless of the difference in fees assessed in various geographical regions, I have noticed that there is bad news and worse news! The bad news is the combined total fee for a tooth requiring endodontics and restorative treatment is "several hundred dollars" less than the total fee assessed for alternative treatments. This sobering revelation is heightened by worse news: Clinicians typically spend more chairtime performing these combined procedures compared to the alternative. My message should be clear. Procedure vs. procedure, you`re spending more time to make less dollars when performing combined procedures, compared to the alternative procedures.
Clearly, this time and fee discrepancy needs to be addressed. A progessive business plan balances the equation once implemented. If the prognosis for endo-restorative is excellent, what dentist would vote for an extraction and follow-up alternative treatment (such as a bridge), which frequently contributes to future endodontics on one of the abutment teeth? Successful endodontic treatment is, at times, tedious, requires precision, and demands specific technology, which gives you permission to charge a fair fee that will empower you to deliver quality and value for your patients.
7. Nonsurgical retreatment
On the other hand, let`s consider the fees for nonsurgical retreatment. But, first, remember that the increase in endodontic treatment is staggering, and it can be described as being a good news-bad news dilemma. The good news is that hundreds of millions of teeth have been salvaged through combinations of endodontics, periodontics, and restorative dentistry. The bad news is that tens of millions of teeth are endodontically failing for a variety of reasons.
To support this assertion, consider the number of articles that have reported endodontic success rates ranging from 53 to 95 percent. This startling range can be attributed to a variety of factors, such as number of treated cases, tooth type, operator ability, limited follow-up periods, and all the clinical-treatment factors that ultimately will influence success or failure. Even if it is assumed that 90 percent of all endodontics works over time, the reciprocal failure rate is 10 percent. Ten percent of the number of cases treated in any given year is a phenomenal number of teeth! If one considers the total number of cases treated during the past three to four decades - when we knew less - the number of failed cases was massive and in the tens of millions.
Endodontic surgery is still too often selected to resolve failures. Even with the vast improvements achieved in surgical endodontics in recent years, surgery still is limited in its ability to predictably eliminate pulp, bacteria, and related irritants from the root-canal system.
Many significant advantages result when failing endodontic cases are nonsurgically re-entered. Endodontic failures can be thoroughly evaluated and explored for coronal leakage, mechanical failures, fractures, and missed canals. More importantly, these root-canal systems can be recleaned, shaped, and packed in three dimensions. In fact, many iatrogenic events can be retreated successfully with nonsurgical methods in today`s world of clinical possibilities.
Consultations should be directed towards communicating:
- The critical importance of disassembly.
- The cost of this approach, as compared to less effective treatment choices.
- The improvement in long-term results. If recommending endodontic nonsurgical retreatment, the prognosis should at least equal the prognosis of alternative treatment choices.
Typically, insurance codes only address pulpal extirpation and obturation, along with other limited procedures. In fact, in most instances, there are no insurance codes to take a crown off, remove a core, identify and treat missed canals, eliminate a post, or to remove gutta percha, silver points, paste, and carriers. Additionally, insurance codes do not address blocks, ledges, perforations, and broken instruments. Consequently, if clinicians make a serious effort to treat these clinical challenges, they must dedicate the proper chairtime and set a fee commensurate with the time spent.
In my practice, I quote two fees for endodontic retreatment. One fee is my usual, customary, and reasonable fee I charge for conventional endodontic procedures, regardless of insurance coverage. The second fee is for what I call "endodontic disassembly," which insurance plans do not cover as part of a standard endodontic procedure. With experience, clinicians will begin to appreciate the time required to predictably and safely disassemble a given endodontic failure and the fee necessary to cover this time.
It is critically important that patients understand that the total retreatment fee minus your root- canal treatment fee equals the "disassembly fee." The fee is their responsibility, since it is not generally covered by their insurance carriers.
If one begins to look at the endodontic retreatment and restorative procedures in terms of both expended time and the fee charged for these services, it is a sobering revelation to see how these numbers compare to the time and cost of alternative-treatment plans. It is no wonder that so many teeth are extracted because of insurance compensation tables that favor and promote alternative treatments. The huge game of nonsurgical retreatment is virtually a vacant niche and provides phenomenal possibilities for trained clinicians.
8. Increasing fees
Successful practices invest in office improvements, people, training, technology, equipment, supplies, systems, and structures. These costs are passed on to patients. If a dental office wants to be viable in the marketplace, it must deliver quality, service, and trust.
The eighth financial factor is that systematic fee increases are essential. With practice-overhead percentages escalating, dentists cannot cut their fees and hope to increase their profitability by increasing patient volume.
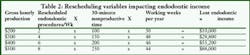
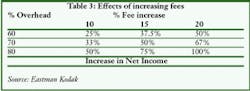
Table 3 shows the relationship between a specific percentage-fee increase and the effect this increase will have on practice profitability at various practice-overhead percentages. For example, a 10 percent fee increase for a dentist whose practice operates with a 70 percent overhead results in a 33 percent increase in practice profitability.
As you can see, the dentist with the highest overhead benefits the most by increasing fees. Traditionally, dentists fear that raising fees will decrease patient acceptance of treatment and ultimately contribute to the loss of market share. I have never met a dentist yet whose practice profitability decreased as a result of a reasonable fee increase.
Most patients will pay your fee if they perceive the value of your service and they receive caring treatment. As you can see, modest fee adjustments make a phenomenal difference for you and provide a pathway for improved quality, satisfaction, and profitability.
9. Coding it medical
Medical insurance can be legally billed, depending on your patient`s medical coverage. Contrary to what you think or have been told, it is legal and your office can submit dental claims for medical coverage in most states, just as speech therapists, chiropractors, home-care providers, optometrists, and podiatrists submit their claims. It is important to recognize that dental and medical insurance is a method of payment, and not a method of treatment. Staff training is essential prior to submitting a dental claim to a medical-insurance company. Office personnel should follow the following steps when submitting a claim:
- You and your patient must never submit to dental first!
- Use medical CPT and ICD-9 codes and not your CDT(ADA) codes.
- Be aware of delays.
- Make sure your state dental board legally will allow dentists to submit medical claims.
- Submit the entire dental procedure to the medical carrier, even if you are sure the medical carrier will deny part of the claim. Separating the procedures performed is called "unbundling" and is illegal.
- Order a good cross-coding book that has done the research for you.
Here are some procedures you can cross-code: anesthesia, supplies, special services, reports, bacteriologic lab services, pathology, office visits, work-related exams, endodontics, periodontics, laser work, oral surgery, implants, orthodontics, temporomandibular disease, and more.
In particular, endodontists can take advantage of this method of billing to save patients` dental benefits for necessary follow-up procedures by the general dentist. When using this venue, train your dental team on the new codes, exercise patience, and work with the medical insurance personnel until they become familiar with your practice and method of billing.
10. Financial policy
Dental practices can increase profitability substantially by unconditionally committing to a sound financial policy - the 10th financial factor discussed in this article.
Many practices realize in-office financing is a lose-lose situation, since a great deal of staff time is devoted to billing and collecting. Several studies have shown that health-care professionals` invoices are the last bills to be paid by consumers due to their shortage of cash. Staff time is better spent impeccably running the practice and business of dentistry, with emphasis on patient relations and marketing.
Many employees are not suited for collections. The stress of collecting shows up in poor performance and high turnover. In many instances, employees inadvertently compromise collections and appear to work more effectively for the patient than their employer. Once the dental team realizes that your office is not a bank for financing patient care, a new written policy can be drafted, integrated, and communicated.
My office has a clear financial policy, and we offer the following options:
- Payment in full upon completion, including a 5 percent discount. The discount is an excellent incentive to encourage patients to pay for their dentistry. Many patients appreciate the savings and will take advantage of the option. Doctors benefit from the immediate cash flow, but they must recognize the 5 percent fee reduction is actually greater since it comes out of the profit margin.
- Major credit card payment in full upon completion. Major credit cards encourage payment, generate immediate income, and help increase treatment acceptance. However, other research has found that the average credit-card holder has a balance within $300 of their available credit. In certain instances, maxing-out a patient`s credit card generates a negative conversation when the card can`t be used for sudden, unexpected, and urgent events. Therefore, an excellent alternative to a major credit card is a "dedicated health-care credit card," which we will discuss shortly.
- Dental and medical insurance. Insurance is a benefit and typically represents a contractual arrangement between patients and their carriers or patients and their employers. The benefit amount varies, is arbitrary, and may or may not cover the procedures performed. It is not wise for dentists to put themselves in the middle between insurance carriers and patients. In my opinion, it is best for patients to pay their entire bills at the time of treatment and be subsequently reimbursed by their carriers. However, for long-standing patients who have demonstrated financial responsibility, you may request they pay at least half of the total fee at the time of treatment, with any remaining balance due upon receipt of payment from the insurance company.
- Dedicated health-care credit card (DHCC). DHCCs are another payment alternative that significantly increases treatment acceptance, cash flow, and patient satisfaction. Many patients either have no available financing or have reached their limits on current credit lines. Most patients are willing to accept more credit debt.
In nearly all instances, DHCCs help practices dramatically increase cash flow for two reasons. More patients are able and willing to accept treatment because they are given long-term payment options. Secondly, DHCC companies pay the practice within the week - sometimes within two business days. The bank does the collections work while you and your staff can focus on serving patients. Financially-arranged dentistry that offers flexible, low-monthly payments is viewed as a value-added service.
DHCC companies generally have competitive rates and convenient terms. CareCredit, for example, offers no initial payment and monthly payments as low as 3 percent of the balance. No-interest, first-time user programs exist to encourage new DHCC customers. DHCCs also give practices a great deal of flexibility. Complete treatment can be scheduled and ideally delivered rather than delaying treatment and scheduling around financial ability.
It is important that you incorporate the DHCC into your marketing strategy. This payment alternative is a benefit to patients, and it should be presented to them in a positive manner. If marketed aggressively, DHCCs can increase your patient base because you are making it convenient for patients to accept treatment. Happy patients make referrals. The staff also must understand the advantages. Some DHCC companies offer training programs and communications materials that help market the payment plan.
Dental practices exist to provide service to patients and to generate profit. Except in rare circumstances, practices should not offer patients interest-free loans. The acceptance of credit cards and the inclusion of a DHCC in your financial policy should have a significant impact on the health of your practice and patients.
A financial policy means the practice gets paid on time, and expenses are kept down, resulting in reduced costs to patients. The staff plays a crucial role in endorsing, communicating, and maintaining your financial policy. Staff members must believe and enthusiastically communicate the value of treatment. Then, set up financial arrangements that move patients into action to invest in their oral health.
11. Fee-for-service vs. managed care
The popularity of the managed-care model has crested due to the public surge of second thoughts, as evidenced by an avalanche of proposals for tighter governmental control. As of this writing, more than 1,000 managed-care bills have been introduced because of a sharp increase in public dissatisfaction. Understandably, countless dentists - who initially embraced managed care programs because of the promise of more patients and greater profitability - are leaving this practice model. The April 1990 issue of the "Blair/McGill Advisory projected the massive number of additional patients and procedures required to offset lost income (Table 4). The possibility of increasing sales to offset decreases in fees to equal the same level of profitability is remote.
As an example, a dentist with a 40 percent profit margin who cuts his fees 10 percent must increase his sales 33 percent to maintain the same level of profitability. However, another colleague who operates on only a 30 percent profit margin must increase sales 50 percent in order to maintain the same level of practice profitability after a 10 percent fee cut.
It should be obvious that increasing patient volume to offset a fee cut means a completely unrealistic volume of patient procedures. The required increase in procedures puts the clinician in imminent danger and shows up in loss of quality, reduced self-esteem, and dislike for what one has dedicated his/her life to do. All this, in concert, takes an immeasurable toll on the professional`s joy, health, and fulfillment.
Fee-for-service will continue to thrive. The model is sustained by the more affluent silver-haired generation that continues to invest in value-based services, as well as a maturing population of "Baby Boomers" who are on the path to economic freedom. Another factor that will drive endodontic demand is the forecast of a critical shortage of dentists beginning in the year 2000.
The future of endodontics is bright, and the demand for initial treatment and retreatment will grow exponentially in the years immediately ahead. Improved concepts, training, and technology will shift endodontic services from "needs" to "wants," as the public increasingly chooses this form of treatment as an alternative to other types of services that are more invasive, less predictable, and more costly. As endodontic treatment fulfills its potential to become quick, painless, and predictable, the discipline will experience a renaissance unparalleled in dental history.
How to scout out DHCC companies
Several DHCC companies are marketing their programs in the dental industry. All of them are different. Here are guidelines to follow when researching the right program for your practice.
- Ensure the company is backed by Fortune 100 financial institutions.
- Determine how long the company has been in the DHCC business.
- A company with a dental background is very helpful.
- Look for a company that is endorsed by dental associations.
- Compare companies` patient approval rates.
- Choose a plan that is nonrecourse (which means that, once the treatment fee is processed through the bank and the practice receives payment, the bank is solely responsible for any failure or delay in payment by the patient).
- Learn what staff training and communications support is offered.
- Confirm that the financial institution will direct-deposit funds into designated accounts.
- Look for a company that offers patient incentives (interest-free programs).
- Compare in-office approval periods. Some approve patients in minutes.
- Check references and discuss with peers.