Creating a culture of safety in dental practice settings
Part one
Mary Govoni, MBA, RDH, CDA
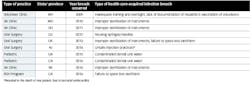
Historically, dentistry in the US has not been associated with high numbers of health-care-acquired infections (HIAs)—that’s the good news.1 The not-so-good news is that recently there have been a number of well-publicized breaches of infection prevention protocols. Some of those breaches led to HIAs, several involving serious consequences and even the death of a patient in the US as a result of an infection acquired during dental treatment.2 (See table 1 for examples of locations and types of breaches.)
These incidents have been investigated by local and state health departments, as well as the Centers for Disease Control and Prevention (CDC), and evidence has revealed that the breaches involved not following standard of care, or recognized safety standards as established by the CDC.3,4 In light of these recent occurrences, and in the interest of increasing safety, there is a new emphasis in dentistry on the oversight of infection prevention and control and general safety in dental settings.
Table 1: Health–care-acquired infection breaches in the United States involving serious consequences
Although the Occupational Safety and Health Administration (OSHA) requires employers to appoint a safety officer or coordinator to oversee the required safety programs that fall under its OSHA General Workplace Safety Standard,5 specifically the Hazard Communication Standard and the Bloodborne Pathogens Standard, many practices do not officially name a safety officer in their written safety plans. The CDC recommends the appointment of an infection control coordinator (ICC)4 to oversee all areas of infection control and prevention to ensure patient and employee safety, while OSHA’s requirement is to promote employee safety. The same team member can serve as the OSHA safety officer and the infection control coordinator, the tasks can be assigned to several team members, or a safety committee can be formed within the practice.
Since the role of an ICC is new to the CDC protocols in the 2016 Summary,4 there may be some questions on the part of the dental team as to how to go about implementing this recommendation. To assist dental practices in accomplishing this, Hu-Friedy has published The Essential Guide to Infection Control e-book available to dental practices as an excellent resource and guide for the ICC and entire dental team (figure 1). The Organization for Safety Asepsis and Prevention (OSAP) also has excellent training resources available at osap.org/page/TrainingResources. In addition, the Dental Assisting National Board (DANB) and the Organization for Safety Asepsis and Prevention (OSAP) are working together to create a credentialing process for dental team members who are serving in the role of the ICC in a dental practice or facility.
Figure 1: The Essential Guide to Infection Control e-book, a resource guide for the entire dental team, is available to dental practices from Hu-Friedy at this link: hu-friedy.com/products/essentialguidetoinfectioncontrolmerged12.
Aside from the training and future credentialing of the ICC in dentistry, there are some other considerations that affect the implementation of this role in a practice. Team members who take on the role of ICC not only will need knowledge of OSHA standards and CDC guidelines, they must also have the support of the doctor(s)/owner(s) of the practice. The doctor/owner must believe that safety is vital to the success of the practice, and safety must be woven into the culture or value system of the practice. To be successful in the role, the doctor/owner or practice administrator must communicate to the entire team that the ICC has the authority to establish and enforce infection control and prevention protocols. In addition, the entire team must be on board with making safety a priority in the practice, not as an afterthought or an irritating regulatory obligation.
Selecting the most appropriate person(s) to fill this need in a practice or facility will depend on the type of practice, size of the facility, size of the team, experience and training level of the team members, and resources available for the ICC. In many cases, the OSHA safety manager is a clinical dental assistant or a practice administrator. Since this is a position that requires great attention to detail, the ICC must have a high level of interest in infection prevention and safety.
The challenge for most ICCs in dental practices, however, is the time needed to develop, document, and maintain the safety and infection control protocols in a practice, while continuing to perform the other functions of their jobs at chairside or managing the practice. This may require additional work hours when patients are not being treated to fully dedicate time and attention to the tasks associated with the ICC role.
The benefit to a practice or facility in implementing the ICC position, or perhaps enhancing the role of the current OSHA safety coordinator, is that patient and employee safety will increase. Costs associated with work-related injuries (especially exposure incidents) can have a very negative effect on the profitability of a practice. If there happened to be an infection control breach that resulted in an infectious disease exposure to patients, the negative publicity and potential downtime in the practice could be even more costly. The bottom line is that close attention to safety is a good business practice.
In Part Two of “Creating a culture of safety in dental practice settings,” we will focus on the specific job description of the ICC and other resources to help practices successfully implement this very important role.
Editor’s note: This article is supported by Hu-Friedy.
References
1. Laheij AM, Kistler JO, Belibasakis GN, Välimaa H, de Soet JJ. European Oral Microbiology Workshop 2011. J Oral Microbiol. 2012;4. doi: 10.3402/jom.v4i0.17659.
2. Epidemiology and prevention of vaccine-preventable diseases: Hepatitis B. Centers for Disease Control and Prevention website. https://www.cdc.gov/vaccines/pubs/pinkbook/hepb.html. Updated March 16, 2017. Accessed December 10, 2017.
3. Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52(RR-17):1-61.
4. Centers for Disease Control and Prevention. Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf. Published October 2016.
5. General Workplace Safety Standard, CFR 1910, Subpart A. Occupational Safety and Health Administration. United States Department of Labor website. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=10109. Accessed December 10, 2017.
Mary Govoni, MBA, RDH, CDA, an internationally recognized speaker, author, and consultant, has worked with teams for more than 40 years on clinical efficiency, infection prevention, and more. A past president and life member of the American Dental Assistants Association, she is a member of the American Dental Hygienists’ Association, Organization for Safety, Asepsis and Prevention, Academy of Dental Management Consultants, National Speakers Association, and Speaking Consulting Network.