What are the main reasons for implant failure?
Q: I have been placing and restoring dental implants for about 10 years. There are times when I feel I have placed an implant nearly perfectly, yet after a short time of adequate service, the implant fails. There have been other times when I could have done a better implant placement, and the implant is successful over many years. There appear to be many reasons for implant failure. What are the most important and common reasons why dental root-form implants fail? Can I avoid these situations and expect more predictable service?
A: I feel the same frustration you have described. Because of these unpredictable surgical situations, I suggest realistically advising those patients considering implants that over 90% of implants serve very well for several years, but some begin to have peri-implantitis or other challenges after approximately 10 years. Patients should be educated about the potential problems that involve implants just as they should be advised about those associated with natural teeth, as well as how to potentially prevent the challenges.
The dental literature is filled with scientific articles suggesting reasons for implant failure and how to prevent failures. I will summarize some of the researched reasons for implant failure and express my own clinical observations on failures I have experienced.
Related reading:
- Is an implant better than a tooth?
- When are implants the best choice?
- Occlusion in 2022: The forgotten area in dentistry
Implant placement for properly diagnosed healthy patients who have adequate bone quantity and quality is a relatively simple procedure that can be accomplished by any dental practitioner who has taken the time to become competent with the procedure. Similar success can be expected with implant restoration.
Implants should be for all patients who need them when all other treatment modes do not appear to be adequate. They are not an equal replacement for a natural tooth and should not be considered as such. However, with proper placement and restoration, implants are an excellent substitute when all clinical conditions are considered.
Every effort should be exerted to retain restorable natural teeth before removing them and placing implants.
Our organization, Practical Clinical Courses, has four levels of implant videos and courses, some of which are described later. Our implant failure course is one of the most popular courses in our 15-course series.
Rather than include all the known potential reasons for implant failure, I will limit this discussion to those I have found to be most significant and commonly occurring. Also, I have not included references for my statements since they are based on innumerous research projects and my own clinical observations over 30-plus years of implant dentistry. Other courses and videos are referenced later in the article.
Occlusion
Smoking
Poor bone
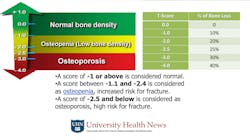
Practitioners can easily see the quantity of bone by observing radiographs, especially cone beam images. However, many dentists do not analyze bone quality or even discuss it adequately with patients. Radiographs can provide hints concerning bone density by allowing observation of the size of bone trabeculations.
If the patient is taking bisphosphonates (Boniva, Fosamax, etc.) as indicated when collecting their diagnostic data, ask what practitioner placed them on the bisphosphonates. Call that practitioner. He or she will usually have completed a T-score test to determine the severity of the bone quality. Usually, the patient will be osteopenic or osteoporotic if taking bisphosphonates (figure 3). It is nearly impossible to significantly increase bone density, although there are a few medications indicated for that use. I suggest considering treating patients whoLoading implants too early
There has been significant marketing for both patients and dentists on “teeth in a day.” Patients and some practitioners see these ads and think that this is always a viable alternative. In some clinical situations, it is an acceptable alternative. However, the clinician accomplishing such treatment must consider all aspects of the clinical situation to determine if perhaps a slower and more predictable alternative would be better for the patient.
What should be considered? Many factors, including patient expectations, bone quantity and quality, long-term prosthesis expectations, esthetics, healing time, ability to predict where soft tissue will heal, occlusion, and so on. Often patients have had missing teeth for a long time. What is the hurry? Slow down and improve the procedure predictability and the long-term service potential. I have had several implant-supported crowns and fixed prostheses fail because of hurrying.
There are a few situations where immediate implant placement is superior to waiting for bone maturity. One of them is in the anterior smile area, where immediate implant placement can often provide better retention of papilla.
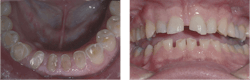
Improper implant placement
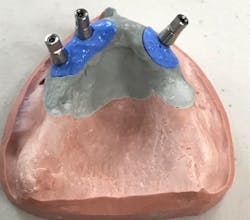
Improper prosthodontic design
Crown and prosthesis planning and design are directly related to anticipated stress to be placed on implants, esthetics, food impactions, open contacts, soft-tissue irritation, and potential implant failure. Dentists should be involved in the details of crown and prosthesis design with laboratory technicians.
Previous periodontal disease
Contrary to previous beliefs, when a patient has had periodontal disease and tooth extraction, the odds of having peri-implantitis later may be increased. In such cases, accomplishing conventional dentistry instead of placing implants orSummary
Although root-form dental implants have been used for more than 30 years and are now popular, in my opinion, we still don’t know more than we know. There are more than 20 factors that allegedly can cause implant failure. Do we really know what causes a specific implant to fail? Not often. This article includes the observational and research views of a prosthodontist who has succeeded and failed with implants for more than 30 years. These observations include some of the most important causes for implant failure. But there are many more reasons!
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic for you and your staff.
One-hour videos:
- The Best Implant-Supported Restorations (Item #V2333)
- Uncomplicated Occlusal Equilibration (Item #V3105)
- Diagnosis and Treatment of Failing Implants (Item #V2391)
Two-day hands-on courses in Utah:
- Avoiding Implant Failures and How to Treat Them with Jon Suzuki, Kevin Suzuki, and Gordon Christensen
- Implant Surgery – Level 1 or Level 2 with Gordon Christensen
For more information, visit our website at pccdental.com or contact Practical Clinical Courses at (800) 223-6569.
Editor's note: This article appeared in the May 2022 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.