Improved efficiencies in implant dentistry: Use of patient-specific accelerated therapy to drive practice growth
Dental implant therapy has been growing steadily over the last several decades. However, the penetration rate of implants within the overall tooth replacement market remains relatively low. This has been driven by factors such as clinician education, increased costs of surgical/restorative procedures, limited insurance coverage, and the extended length of time associated with treatment. The implant industry has responded to these hurdles by offering value brands that mitigate some of the challenges. Although competitive pricing is helpful, it may lead to the use of inexpensive and/or poorly designed implants in cases where more advanced designs are indicated. A short-term windfall can easily turn into financial and clinical challenges.1-3
Site-specific implants for specific and varied implant surgical and prosthetic therapies allow clinicians’ choices regarding precisely designed products for individual clinical applications. These implants have been developed to provide improved primary stability, avoid/minimize preimplant bone grafting procedures, and allow for improved soft- and hard-tissue preservation around implants.4,5 Site-specific implants can also accelerate treatment by placing specific implants directly into extraction sockets immediately after tooth removal. Furthermore, if primary stability is optimized, site-specific implants can be loaded sooner, which usually leads to fewer patient visits, better soft-tissue profiles, and quicker overall treatment.5-9
Screw- versus cement-retained implant restorations
Cacaci et al. recently published the results of a clinical study that compared the performance of screw- versus cement-retained implant restorations.10 After a mean clinical service time of 36.9 months, porcelain veneer fractures occurred in 1.8% of the cases. The authors concluded that the type of retention did notEarlier, Vigolo et al. reported the results of a 10-year clinical study that compared screw- versus cement-retained crown restorations.12 They concluded that there was no evidence of significant differences in clinical parameters of peri-implant marginal bone or peri-implant soft tissues with either cement- or screw-retained single-tooth implant restorations.
Excess subgingival cement has been associated with increased incidences of peri-implant mucositis and peri-implantitis. Screw retention has an added benefit in that cement is not used, so it cannot be left behind.
Staubli et al. published a systematic review regarding excess cement and the risk of peri-implant disease.13 They concluded that excess cement was a possible risk indicator for peri-implant diseases and was more frequently observed with soft-tissue healing periods shorter than four weeks. To reduce the risk of peri-implant disease associated with excess cement, supragingival crown margins were recommended.
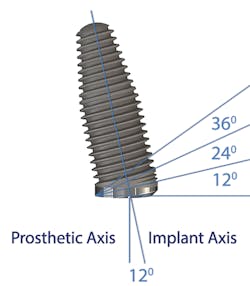
Author Gary Morris, DDS, tracked the paradigm shift from cement- to screw-retained implant restorations in his clinical prosthodontic practice. This was directly related to the introduction of angled implants (Co-Axis Implants, Southern Implants; figure 1). Co-Axis Implants were designed with angle offsetsGrowth of simultaneous extraction and molar implant placement
The authors noted a paradigm shift in their practices over the last several years. Hattingh et al. published a technique article regarding immediate placement of ultrawide diameter implants in molar sockets.14 Instead of the more traditional protocol that involved diagnosis of a nonrestorable molar with subsequent extraction, graft, osseous healing, implant placement, osseointegration, and implant restoration, the authors adopted an accelerated treatment protocol due to the availability of site-specific implants.
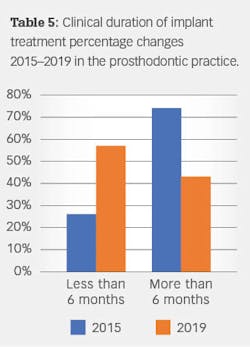
The original protocol generally required 6–18 months for patients to receive implant-retained restorations. The accelerated treatment protocol typicallySingle-/multiple-unit/full-arch treatment with and without immediate occlusal loading
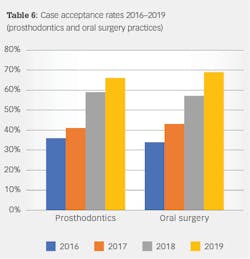
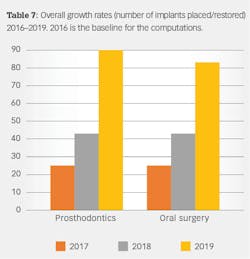
Anatomical constraints at implant sites often present a conflict between surgical and prosthodontic prerequisites for screw-retained implant-supported prostheses. Howes published the use of a dual-axis implant designed to help clinicians overcome these challenges by facilitating accurate surgical placement and prosthetic simplicity, as well as improved biomechanics and enhancedSince the authors have adopted accelerated treatment protocols with site-specific implants, they both have noted increased acceptance rates, as well as growth in implants placed and restored. Table 6 illustrates the increased acceptance rate for implant treatment in both practices. Data reflects patient acceptance of implant treatment at the first consultation/clinic visit.
The authors correlated the increased acceptance rates with several factors, including consistent, well-manufactured, precise implant and restorative components; multiple implant choices that fit a multitude of clinical situations;Summary
The science and clinical implementation associated with implant dentistry have changed over the past several decades. Likewise, the authors have also modified and adapted their clinical practices to incorporate innovations into theirAs innovations continue in implant dentistry, change is the only constant. Clinicians and manufacturers will need to continue clinical and laboratory research to meet the ongoing challenges of dentate and edentulous patients.
Authors’ disclosure: Drs. Morris, Steinberg, and Drago are spokespersons for Southern Implants North America. Products mentioned in this article are used inReferences
- Goodacre BJ, Goodacre SE, Goodacre CJ. Prosthetic complications with implant prostheses (2001–2007). Eur J Oral Implantol. 2018;11(Suppl 1):S27-S36.
- Romanos GE, Delgado-Ruiz R, Sculean A. Concepts for prevention of complications in implant therapy. Periodontol 2000. 2019;81(1):7-17. doi:10.1111/prd.12278
- De Kok IJ, Duqum IS, Katz LH, Cooper LF. Management of implant/prosthodontic complications. Dent Clin North Am. 2019;63(2):217-231. doi:10.1016/j.cden.2018.11.004
- Östman PO, Chu SJ, Drago C, Saito H, Nevins M. Clinical outcomes of maxillary anterior postextraction socket implants with immediate provisional restorations using a novel macro-hybrid implant design: an 18- to 24-month single-cohort prospective study. Int J Periodontics Restorative Dent. 2020;40(3):355-363. doi:10.11607/prd.4467
- Chu SJ, Tan-Chu JHP, Levin BP, Samachiaro GO, Lyssova V, Tarnow DP. A paradigm change in macro implant concept: inverted body-shift design for extraction sockets in the esthetic zone. Compend Contin Educ Dent. 2019;40(7):444-452.
- Chen ST, Wilson TG Jr, Hämmerle CHF. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19(Suppl 1):12-25.
- Walker LR, Morris GA, Novotny PJ. Implant insertional torque values predict outcomes. J Oral Maxillofac Surg. 2011;69(5):1344-1349. doi:10.1016/j.joms.2010.11.008
- Vandeweghe S, Ackermann A, Bronner J, Hattingh A, Tschakaloff A, De Bruyn H. A retrospective, multicenter study on a novo wide-body implant for posterior regions. Clin Implant Dent Relat Res. 2012;14(2):281-292. doi:10.1111/j.1708-8208.2009.00253.x
- Al-Sabbagh M, Kutkut A. Immediate implant placement: surgical techniques for prevention and management of complications. Dent Clin North Am. 2015;59(1):73-95. doi:10.1016/j.cden.2014.09.004
- Cacaci C, Cantner F, Mücke T, Randelzhofer P, Hajtó J, Beuer F. Clinical performance of screw-retained and cemented implant-supported zirconia single crowns: 36-month results. Clin Oral Investig. 2017;21(6):1953-1959. doi:10.1007/s00784-016-1982-1
- Weigl P, Saarepera K, Hinrikus K, Wu Y, Trimpou G, Lorenz J. Screw-retained monolithic zirconia vs. cemented porcelain-fused-to-metal implant crowns: a prospective randomized clinical trial in split-mouth design. Clin Oral Investig. 2019;23(3):1067-1075. doi:10.1007/s00784-018-2531-x
- Vigolo P, Mutinelli S, Givani A, Stellini E. Cemented versus screw-retained implant-supported single-tooth crowns: a 10-year randomised controlled trial. Eur J Oral Implantol. 2012;5(4):355-364.
- Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of peri-implant disease – a systematic review. Clin Oral Implants Res. 2017;28(10):1278-1290. doi:10.1111/clr.12954
- Hattingh AC, De Bruyn H, Ackermann A, Vandeweghe S. Immediate placement of ultrawide-diameter implants in molar sockets: description of a recommended technique. Int J Periodontics Restorative Dent. 2018;38(1):17-23. doi:10.11607/prd.3433
- Howes D. Angled implant design to accommodate screw-retained implant-supported prostheses. Compend Contin Educ Dent. 2017;38(7):458-463.
- Schnitman PA, Wöhrle PS, Rubenstein JE, DaSilva JD, Wang NH. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12(4):495-503.
- Chen J, Cai M, Yang J, Aldhohrah T, Wang Y. Immediate versus early or conventional loading dental implants with fixed prostheses: a systematic review and meta-analysis of randomized controlled clinical trials. J Prosthet Dent. 2019;122(6):516-536. doi:10.1016/j.prosdent.2019.05.013
- Drago C. Cantilever lengths and anterior-posterior spreads of interim, acrylic resin, full-arch screw-retained prostheses and their relationship to prosthetic complications. J Prosthodont. 2017;26(6):502-507. doi:10.1111/jopr.12426
- Jensen OT, Ringeman JL, Adams MW, Gregory N. Reduced arch length as a factor for 4-implant immediate function in the maxilla: a technical note and report of 39 patients followed for 5 years. J Oral Maxillofac Surg. 2016;74(12):2379-2384. doi:10.1016/j.joms.2016.08.002
- Crespi R, Capparè P, Gastaldi G, Gherlone EF. Immediate occlusal loading of full-arch rehabilitations: screw-retained versus cement-retained prosthesis. An 8-year clinical evaluation. Int J Oral Maxillofac Implants. 2014;29(6):1406-1411. doi:10.11607/jomi.3746
GARY MORRIS, DDS, received his dental degree from the University of Illinois at Chicago and did his residency in prosthodontics at the UMKC College of Dentistry in Kansas City, Missouri. He is an adjunct clinical assistant professor at Southern Illinois University School of Dental Medicine and a member of several dental organizations. A frequent author, Dr. Morris has lectured extensively nationally and internationally on implant prosthodontics. He maintains a private practice limited to prosthodontics and restorative dentistry in Buffalo Grove, Illinois.
MARK J. STEINBERG, DDS, MD, FACS, received his dental degree from Northwestern University School of Dentistry and later earned an MD degree from Hahnemann University School of Medicine in Philadelphia. He is board certified by the American Board of Oral and Maxillofacial Surgery. Dr. Steinberg maintains an academic appointment as clinical professor of surgery at Loyola University Medical Center in addition to a private practice with offices in Northbrook and Lake Forest, Illinois.
CARL DRAGO, DDS, MS, FACP, received his dental degree from the Ohio State University College of Dentistry. He is an adjunct associate professor in graduate prosthodontics at Marquette University School of Dentistry and maintains private practices limited to fixed, removable, and implant prosthodontics in Brookfield and West Allis, Wisconsin. A diplomate of the American Board of Prosthodontics, he has written five textbooks on dental implants and lectured nationally and internationally. Dr. Drago is a reviewer for the Journal of Prosthetic Dentistry and assistant section editor for the Journal of Prosthodontics.
About the Author

Gary Morris, DDS
GARY MORRIS, DDS, received his dental degree from the University of Illinois at Chicago and did his residency in prosthodontics at the UMKC College of Dentistry in Kansas City, Missouri. He is an adjunct clinical assistant professor at Southern Illinois University School of Dental Medicine and a member of several dental organizations. A frequent author, Dr. Morris has lectured extensively nationally and internationally on implant prosthodontics. He maintains a private practice limited to prosthodontics and restorative dentistry in Buffalo Grove, Illinois.

Mark J. Sternberg, DDS, MD, FACS
MARK J. STEINBERG, DDS, MD, FACS, received his dental degree from Northwestern University School of Dentistry and later earned an MD degree from Hahnemann University School of Medicine in Philadelphia. He is board certified by the American Board of Oral and Maxillofacial Surgery. Dr. Steinberg maintains an academic appointment as clinical professor of surgery at Loyola University Medical Center in addition to a private practice with offices in Northbrook and Lake Forest, Illinois.

Carl Drago, DDS, MS, FACP
CARL DRAGO, DDS, MS, FACP, received his dental degree from the Ohio State University College of Dentistry. He is an adjunct associate professor in graduate prosthodontics at Marquette University School of Dentistry and maintains private practices limited to fixed, removable, and implant prosthodontics in Brookfield and West Allis, Wisconsin. A diplomate of the American Board of Prosthodontics, he has written five textbooks on dental implants and lectured nationally and internationally. Dr. Drago is a reviewer for the Journal of Prosthetic Dentistry and assistant section editor for the Journal of Prosthodontics.