Driving medical-dental integration with telehealth technology
Despite almost a decade of discussion about medical-dental integration, the delivery of oral health care and systemic health care is still largely done in parallel. Numerous studies show that having separate health-care systems treating the same patients results in poor health-care outcomes and high health-care costs.
Mountains of evidence and high visibility have done little to bridge the gap. Why? Because it is a complex problem.
It was initially thought that the solution would be to colocate medical and dental facilities where primary care medical services could be provided during dental appointments, especially for patients with chronic diseases. It would be convenient for a nurse to draw blood for lab tests, review medications, and more while a patient is in the dental chair.
Colocation can be a good start, but some big problems still need to be addressed.
What should be addressed
- Integrated patient care requires much more than just being next door. Common ways and means of collaboration need to be established; i.e., who does what, when, and how.
- Who pays? Financing for integrated service delivery is almost nonexistent, and the third-party reimbursement systems for medical and dental could not be more disparate. Intuitively, the savings realized from the health-care financing system combined with the current spend on dental should suffice, but right now there is very little being done to solve the problem.
- Logistically, how will the approximately 100,000 stand-alone dental facilities in the US colocate with medical facilities? It is unreasonable to assume that colocation will move at anything other than a snail’s pace.
- Medical and dental records need to be integrated. Even with other barriers removed, the lack of focused collaborative software technology could hinder integrated treatment efforts. In fact, information technology limitations have been shown to be the reason for the exclusion of dental benefits from many accountable care organizations.
Because of recent collaboration tools developed within telehealth technologies, the solutions to these problems may not be as insurmountable as they seem. Allow me to share an example that is hypothetical as of this writing, but active discussions with accountable care organizations (ACOs) are underway.
ACOs want to offer limited but very important dental benefits. They recognize the patient health benefits and health-care cost savings of delivering preventive dental care to those with diabetes and periodontal disease. As part of its health-care benefit offering, these patients receive preventive dental services performed at ambulatory health-care clinics at no charge.
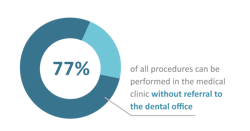
Rather than build and staff a dental facility in the medical clinic, an ACO reaches an agreement with a local dentist to oversee a hygienist who will perform services in the medical facility. The hygienist uses a mobile cart and mobile equipment in any open room at the facility for the day.
The hygienist screens all patients with diabetes and gathers appropriate diagnostic records (x-rays, images, charting) into the dental electronic health record (EHR), which is a component of the telehealth software. The dentist then reviews the records, typically within 24 hours (asynchronous). If the hygienist decides it’s necessary to do an immediate consultation with the dentist (perhaps to view a lesion via an intraoral camera), a secure videoconference (synchronous) can be done on the spot.
Once it is determined that a patient is eligible for the benefit, the hygienist becomes the care coordinator by collaborating with a nurse, physician, etc., before each dental appointment. The result is an integrated delivery model that takes advantage of every single patient touch point. This makes care more convenient for the patient and for training doctors and nurses to work outside of their traditional areas to provide the best care.
What is telehealth technology?
Critical to the success of this model is the telehealth technology platform that facilitates easy collaboration and communication among all parties: patients, hygienists, physicians, nurses, and any other health-care workers.
Telehealth technology is often thought to be simply secure videoconferencing. The platform required to support this model is significantly more sophisticated. Yes, it offers secure videoconferencing, but it takes telecommunications much further. It seamlessly enables 1) functionality for superior patient engagement, or more broadly, patient participation in their health care; 2) easy multidisciplinary collaboration, record sharing, and monitored continuity of care; 3) interchangeable EHRs that vary depending on the primary user’s specialty or subspecialty; and 4) a subset of the shared data into the appropriate applications; e.g., a dentist’s practice management application as shown in Figure 2.
To summarize, colocation of medical and dental facilities is one approach to facilitate medical-dental integration, but it is not the only one. The value of colocation is that collaboration is seemingly easier, and certainly the ways and means of collaboration are key. Physical proximity is helpful in collaboration, but with it is not neccesary with new telehealth technologies.
The hypothetical case presented occurs when a dental hygienist performs preventive services and collects diagnostic records in a medical facility. Working with a remote dentist, the hygienist can act as a care coordinator to bring together dentist, physician, and other health-care workers as needed by using sophisticated EHR-enabled telehealth technology.
Reference
1. Solomon ES. The future of dental practice: Demographics. Dental Economics. April 10, 2015. https://www.dentaleconomics.com/practice/article/16391631/the-future-of-dental-practice-demographics
WILLIAM JACKSON, DDS, is the cofounder and COO of Virtual Dental Care Inc., a telehealth technology company founded in 2016. The company’s flagship software, Teledentix, helps clients such as Onsite Dental, Virtudent, and Arch Orthodontics increase patient participation and streamline communications. Online appointment booking, virtual visits, referrals, and networking capabilities are some of the tools offered by Teledentix. For more information about Teledentix or to contact Dr. Jackson, visit get.teledentix.com or email [email protected].
About the Author

William Jackson, DDS
WILLIAM JACKSON, DDS, is the cofounder and COO of Virtual Dental Care Inc., a telehealth technology company founded in 2016. The company’s flagship software, Teledentix, helps clients such as Onsite Dental, Virtudent, and Arch Orthodontics increase patient participation and streamline communications. Online appointment booking, virtual visits, referrals, and networking capabilities are some of the tools offered by Teledentix. For more information about Teledentix or to contact Dr. Jackson, visit get.teledentix.com or email [email protected].