Preventing recurrent dental caries
Q: I am concerned about the short life expectancy of some of my dental restorations. I have been practicing for 25 years and have had the opportunity to see some of my restorations last for that same period of time. Some look very good after many years, but others have caries around them after only a few years. This situation does not occur only with composite restorations. Some of my crowns also fail prematurely. Can you provide some potential reasons for recurrent caries and suggest what I can do to prevent this problem?
A: As you know, some patients think that dental restorations should last a lifetime, and they are upset if a restoration fails. We dentists are also frustrated when our treatment fails. In this brief answer for you, I will provide both research and clinical observations that may help you in determining what to do about this problem. I will consider composite resin, amalgam, and crowns in that order.
Resin-based composite
Bonds are transient—To make this statement clearer, consider your removal of a failing ceramic veneer, such as feldspathic or IPS e.max (Ivoclar Vivadent), from a bonded prep that was all on dentin versus a bonded prep that was cemented over enamel. The veneer that was “bonded” to enamel was almost impossible to remove, while the one “bonded” onto dentin was very easily removed. Why? The ceramic veneer on enamel had hydrofluoric acid etching on its internal surface, and the enamel that was etched with phosphoric acid had millions of irregularities on its surface. The result is that the ceramic veneer was luted to the enamel, and it could not come off without significant effort. The veneer on dentin soon lost its retention due to expansion and contraction related to the hot and cold foods and beverages the patient ingests.
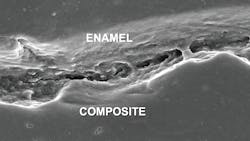
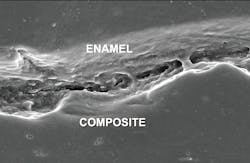
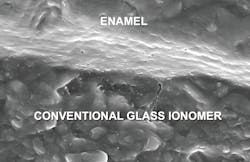
What is the obvious conclusion? Resin-based composite restorations are not sealed, and the tooth preparations contain billions of organisms that must be killed before placing restorations. If this is not done, subsequent caries (usually called recurrent caries) is really continuing caries. Kill the organisms. Additionally, use conventional glass ionomer as a dentin substitute in deep preparations and where cariostatic activity is needed.
Amalgam
Will the arguments about the alleged toxic effects of amalgam ever cease? In spite of support from the American Dental Association, many other national dental organizations, and the World Health Organization, amalgam has many opponents. Nevertheless, surveys show that most American dentists use amalgam at least some of the time. Amalgam is well known to serve up to twice as long as composite in similar-sized tooth preparations.
What are the possible reasons? Contrary to composite, most amalgams expand slightly during service, and corrosion of the metals in amalgam provides much better marginal adaptation and seal than composite. Additionally, amalgam contains several elements, including silver, tin, copper, zinc, other trace elements, and mercury. Some of these elements have cariostatic properties.
What can you do to reduce the continuing caries when using amalgam? Use a careful clinical technique and the same glutaraldehyde procedure as described for composite resin, followed postoperatively by routine use of high-fluoride-containing (5,000 ppm) liquids, gels, or toothpastes for patients with high caries activity. Colgate 5,000 ppm fluoride-containing products are proven to be effective.
Crowns
Crowns are much more expensive than composite or amalgam restorations. When teeth having crowns become carious, patients are justifiably frustrated. The main aspects of crowns that I will focus on are cements and cementation. In the past, zinc phosphate and glass ionomer were the primary cements. With the exception of frequent postoperative tooth sensitivity, these cements had few problems. Both have been used with success for millions of crowns.
In recent years, resin and resin-modified glass ionomer cements have dominated crown cementation, and crown materials have changed from porcelain-fused-to-metal (PFM) and full-metal to ceramic, which includes zirconia. Currently, crowns coming off in service is a major problem with zirconia and less of a problem with lithium disilicate, the two most popular crown types.
Why are crowns developing caries on their margins? A major reason is allowing moisture contamination on the crown margins during cementation. Another is the fact that the majority of current milled crowns have significantly more open margins than the metal crowns of the past, allowing more potential leakage and ingress of food debris and organisms.
What can be done to reduce the possibility of caries occurring on crown margins? When possible, the use of cariostatic cements is a must. The most popular brands are RelyX Luting Plus (3M) and FujiCEM Evolve (GC America) resin-modified glass ionomers. Both of these cements and other brands have a few-second tack cure feature, which reduces the opportunity for salivary and other moisture contamination at the time of seating.
Again, I recommend using the glutaraldehyde disinfecting and desensitizing technique described earlier at the time of cementation or both immediately after prepping the tooth and at cementation.
Careful clinical techniques
Seating crowns might seem like an easy procedure to some dentists. However, many consider it one of the more demanding procedures. Cements may easily become contaminated when seating if extreme care is not taken to clean the tooth of debris, disinfect the tooth, and avoid salivary and blood contamination.
Summary
Dental caries is a preventable disease, but most patients eat caries-promoting foods and do not accomplish oral hygiene adequately. The result is recurrent, or what I call continuing, caries on composites, amalgams, and crowns. Careful clinical techniques help to reduce continuing caries. Use of glutaraldehyde disinfecting and desensitizing products before restoring tooth preparations is highly advised. Using conventional glass ionomer as a dentin-replacement material in deep preparations is advised. Using high-fluoride-containing preventive products postoperatively on a routine basis is suggested for patients with high caries activity. Patients deserve our best restorative dental treatment, and the procedures described in this article will help to achieve that goal.
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic for you and your staff.
One-hour videos:
• Making Foolproof Class II Restorations (Item V3501)
• Foolproof, Fast, Single-Crown Procedure (Item V1980)
Two-day hands-on courses:
• Restorative Dentistry 1—Restorative/Esthetic/Preventive with Dr. Gordon Christensen
• Restorative Dentistry 2—Fixed Prosthodontics with Dr. Gordon Christensen
For more information about these educational products, call (800) 223-6569 or visit pccdental.com.
About the Author

Gordon J. Christensen, DDS, PhD, MSD
Gordon J. Christensen, DDS, PhD, MSD, is founder and CEO of Practical Clinical Courses and cofounder of Clinicians Report. His wife, Rella Christensen, PhD, is the cofounder. PCC is an international dental continuing education organization founded in 1981. Dr. Christensen is a practicing prosthodontist in Provo, Utah.