Perio Aware
When do we become perio savvy? And if you’re not, why not?
When do dental practitioners become perio aware? I mean really aware? Yes, we all took the periodontics courses in dental school and performed the obligatory scaling and root planing to pass our boards, but how many times do we consider periodontics before we look at restorative needs? According to the U.S. Surgeon General’s Report on Oral Health 2000, 85 percent of adults over age 18 are affected by periodontal disease. We would like to think all practitioners consider the foundation prior to restoring the structure. But, do we?
Let’s take a trip down memory lane. Think back to dental school. We had to take a series of coursework to prepare for patient care. Mannequins and dentecs became our friends (if not our mobile, uncompromised patients). We scaled on plastic root structure and sometimes on extracted teeth. We were meticulous (and very slow) while probing each other, only to find barely three millimeter sulcular depths. But, in addition to our diligent probing, we were also setting plastic teeth, carving wax, and learning about the biochemistry of gypsum crystals.
Progressing into the clinical program, we were assigned a group of patients with a list of requirements or tasks essential to graduate. Regardless of the methods of assessment and numbers of procedures necessary, all students go through the process of treating the complete patient. Treatment planning and comprehensive care for all patients are in preparation for the boards required to gain licensure in a state or region. Additionally, these skills are the basis for the standard of care when we leave the educational setting and enter professional practice.
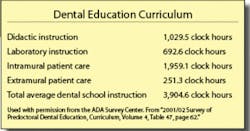
The American Dental Association Accreditation Standards for Dental Education programs do not detail how many specific courses, instructional hours, or clinical experiences a dental education program must present in periodontics. Although, according to the 2001/2002 Survey of Predoctoral Dental Education, the mean number of didactic clock hours in periodontics is 65.4, laboratory instruction is 25.7, and patient care is 239.2, for a total mean of 295.8 clock hours of instruction in periodontics. Considering that the entire dental school program consists - on an average - of 3,904.6 hours of total instruction, periodontics is about 7 percent of the curriculum. This statistic doesn’t diminish the importance of this huge component of our professional practice, but does it predict future focus?
After dental school came the beginning of our real dental lives. How much of that intricate probing that we learned in school are we still performing? In practice, we are faced with a patient in our chair who appears with a bevy of dental issues, not only periodontal disease. Are the periodontal needs of our patients fully addressed, or do we allow some of the probe readings to slip away in lieu of restorative care? Again, don’t we need that solid foundation prior to building the house?
Sometimes, in the course of our busy practices, we may treat the broken tooth or place the full-coverage restoration prior to considering the underlying support. No, this isn’t the correct way to treatment plan, but when faced with pain, esthetic concerns, or loss of tooth structure, the restoration may come before the treatment of burgeoning periodontal disease. We may also delegate periodontal patients to our hygienists, only giving a cursory check and a quick hello, while running to the next treatment room to restore an implant or place a permanent fixed prosthesis.
Periodontal disease is a true infection, creating a full inflammatory response in reaction to the stages of the disease. I heard someone say that if a patient were bleeding from the ear, he or she would rush to the hospital emergency room, probably ignoring stop signs! But when a patient’s gingival tissue is hemorrhagic, he or she doesn’t seem to care. Could it be because we fail to focus on the underlying infection, and merely recommend an increase in flossing or brushing to remove the plaque? We need to adjust our priorities so that we concentrate our attention on our patients’ periodontal needs.
Let’s focus on the infection. We know that periodontal disease is caused by bacteria (primary etiology). Genetics will determine the susceptibility and resistance of the host (gingiva). Genetics will modify the host reaction to the bacterial attack. Different people are affected in different ways. A person with a strong set of genetics and excellent home care may have gingival issues from certain medications. Another person with horrible genetics (poor host resistance) may do everything correctly and still suffer from periodontal disease. So, genetics is really the ballpark where everything happens. Hormones (puberty, pregnancy), stress, medications, systemic diseases (diabetes specifically but many others), and poor nutrition are the players in the ball field. They all influence how the body reacts to the bacterial attack.
We know the plaque biofilm begins innocuously as nonpathogenic, normal intraoral bacteria, which forms almost immediately after brushing, flossing, and dental prophylaxis. This is not a commercial for “Well, if it forms immediately, then aren’t we in a losing battle, so why bother?” Absolutely not. The matrix can be disrupted by home and professional care, so that is why we need to bother. We need to reinforce the need for our patients to perform daily home care. The later entrants in this biofilm collection are the anaerobic players that cause the destruction and inflammation. These anaerobes are the nasty pathogens that cause the most damage inside the sulcus. Remember, they can’t go out to eat, so they survive in their own little world - the protected sulcus. Depending on the depth of the sulcus, they have unlimited party space and limitless ability to do damage to the bone and supporting structures.
Current research has shown a relationship between periodontal diseases and diabetes, cardiovascular disease, stroke, and adverse pregnancy outcomes such as preterm births and low-birth-weight babies. This relates to the inflammation component of periodontal disease. Periodontal disease is an infection that sets off an inflammatory response. The bacteria in the biofilm release several products, such as lipids, proteins, and acids, that will stimulate osteoclastic activity. This will not only cause the destruction of the bone tissue, but will trigger an immune response in the body. As a component of the immunological cascade response, the liver triggers C-reactive protein to be released. An elevated CRP causes an increase in cardiovascular incidents, such as heart attacks and strokes.
With all of this information, why are we not focusing on the periodontal health of every patient? Every patient has probe readings as part of his or her initial comprehensive oral evaluation and routine preventive maintenance. We need to be proactive and diligent in our oral hygiene instructions to patients. In most offices, this task is relegated to the hygienist. But as dentists, we must spend more than a few minutes at each periodic evaluation discussing the importance of home care to stress the connection between the plaque and the inflammation. The message is stronger coming from the entire team.
Several companies are making life easier for us in explaining home care and the reasons why we need to improve oral hygiene to improve not only the oral conditions, but systemic health as well. Johnson and Johnson has “Flossing Matters - Bringing Out the Flosser in Every Patient.” This unbranded, dual set of materials (one for the patient and one for the professional to use at chairside) discusses oral care to patients, based on specific age groups, and offers suggestions to practitioners on how to motivate patients to floss. OraPharma has a patient-centered brochure about asking for “numbers,” or periodontal probe readings. OraPharma’s new educational materials make it easy for dental professionals to explain to their patients that periodontal disease is a chronic oral infection. This campaign will be extremely useful in increasing patients’ knowledge of periodontal disease, making the dental professional’s job of diagnosing and treating this prevalent disease much easier. The ADA has other unbranded materials available for the “show and tell” portion of patient education.
Considering treatment options for periodontal disease, we have several surgical and nonsurgical approaches available. Often, patients in need of scaling and root planing go unscheduled. Whether it is due to time constraints, insurance issues, cost, or believing the patient “won’t understand the need,” we have to discuss the ramifications of unchecked periodontal disease with patients and educate them toward a proper treatment regime. Pregnant women need to be educated about the importance of effective home care. Numerous recent studies have attributed women with periodontitis seven to eight times more likely to have a preterm or low-birth-weight baby. Cardiac patients also need to be educated about the risk of periodontal disease and increases in their circulating CRP levels.
In addition to mechanical scaling and root planing, adjunct therapies are very beneficial. Some practitioners use systemic antibiotics, singly or in combination, for a specific regimen. Antimicrobial mouth rinses, such as Periostat, or other chlorhexadine preparations are also available. Finally, since scaling and root planing alone cannot reach the base of all pockets, newer locally applied antibiotics (LAA) that offer precise placement of the drug directly into the sulcus are also excellent therapies. Again, referencing the Surgeon General’s Report on Oral Health, “antimicrobial agents [are placed] directly into the pocket. Antimicrobials incorporated into either resorbable or nonresorbable interpocket delivery systems have been studied in randomized, double-blind, controlled clinical trials and are now FDA-approved and on the market (Goodson et al. 1991, Jeffcoat et al. 1998). When used as an adjunct to scaling and root planing, gains in clinical attachment level and decreases in probing depth and gingival bleeding were demonstrated.”Three such very effective products are Arestin, Atridox, and PerioChip. They are placed by either the dentist or dental hygienist.
Now, let’s get to the bottom line. According to Dr. Gordon Christensen at a recent lecture, dentists may be missing 10 percent of our periodontal treatments. It is not that we aren’t properly diagnosing, but we may have another 10 percent of our patients who need active periodontal treatment. If we are not treating this segment, for whatever reason, then we are, in effect, losing money. By increasing the necessary periodontal treatment of our patients, we will always increase the bottom line (and make those accountants happy). It isn’t as if we are looking for things to do; the periodontal issues are most likely there and available to treat by either the dentist or the hygiene team.
Consider this: the most recent Dental Economics® fee review stated that scaling and root planing (4341) would generate an average of $210 per quadrant, depending on the area of practice. Chemotherapeutic agent placement (4381) ranges from $40 to $50 per tooth. Adding a few patients per week in the hygiene schedule will produce revenues of a minimum of $3,000 per week. Since I was not a math major in school, extrapolate that out to a 40-week year (and most of us do work more than 40 weeks in our hygiene department), this will translate to more than $120,000 a year. And getting patients to accept this additional treatment, as well as your entire plan for comprehensive care, is now easier due to the wide availability of patient financing programs. These companies have a wide variety of plans for your patients to choose from, including no interest and long-term payment plans. Look for a revolving line of credit that can be used for subsequent treatment or other family members. The CareCredit program has been integrated into several desktop software programs so your staff can submit applications from the front desk or operatory, while your patient is still in the chair.
Being perio savvy may sound like a no-brainer. At the very least, we are protecting our patients from tooth loss and possible systemic diseases. At best, we are protecting ourselves from a lawsuit. Are you savvy? If not, why not?
The author wishes to thank Dr. Terry J. Annex and Jeff Gartman, reference and online resource librarian from the ADA, for their invaluable support and assistance. References available upon request.
Sheri B. Doniger, DDS, is the editor of Woman Dentist Journal®, a sister publication of Dental Economics®. She has been in the private practice of family and preventive dentistry for more than 20 years. A dental hygiene graduate of Loyola University prior to receiving her dental degree, Dr. Doniger’s current passion is focusing on women’s health and well-being issues. She may be contacted at [email protected].