New techniques for diagnosing oral cancer
New technology helps dentists detect even precancerous lesions so that patients can benefit from life-saving treatment.
Myer Leonard, DDS
More people suffer from oral cancer than suffer from skin cancers or cancers of the uterine cervix. I don`t suppose anyone reading this article would doubt that more women arrange for a regular cervical pap smear test or that more folks consult their dermatologists about moles or keratotic lesions than consult their dentists about worrisome oral lesions.
Obviously, there are reasons for this. You can easily see changes in your skin. A friend or family member might even notice a darkened patch of skin and urge you to consult a dermatologist. I`ve been told that a major part of adult dermatology is checking out "suspicious" patches.
The laudable public health programs which emphasize the need for cervical-cancer checkups have resulted in hundreds of thousands of women getting regular pap smears. In doing this, they are reassuring themselves about the continued health of their tissues, in addition to giving themselves an opportunity for prompt and expeditious treatment if there has been dysplastic change in the tissues.
The dental profession has not been so emphatic in proposing the virtues of regular oral examinations. Again, there are reasons for this. One of them is, undoubtedly, a belief that oral cancer is rare, the lesion will be obvious, not much can be done, and lastly, when the lesion is diagnosed, it usually has advanced too far for life-saving treatment.
These reasons are no longer valid. Oral cancer is uncommon, but not rare. It is not obvious, but much can be done and the diagnosis can be made easily.
Part of our protocol to change our mind-set should be based on the commitment to do a thorough oral examination on every patient every six months to a year. This exam should go beyond recording the cavities and restorations, pocket depths, and missing teeth. You should conscientiously inspect the tongue, the palate, the floor of the mouth, the buccal mucosa, the fauces, etc. This means determing whether all the tissues are normal and healthy. Be sure you explain to the patient what you are checking. A gynecologist would not do a pap smear without informing the patient about the procedure and its purpose.
Telling your patients what you are doing and why you are doing it is an important part of good public relations. The technique described for doing an oral cancer exam is more diagnostic in nature than a pap smear. Doing a thorough oral exam should become part of every dentist`s armamentarium.
Cellular changes
The earliest signs of abnormality in the oral lesion are cellular. The cells, particularly the nuclei, change their shape. These changes are common to dysplasia or precancerous conditions throughout the epithelium. However, in the oral cavity and related epithelium of the nose and throat, additional unique markers of abnormality relate to the early signs of abnormal keritanization. The realization that these changes occur in oral lesions - and that they may be the earliest microscopic signs of an oral cancer - have been known for some time.
The OralCDx computer system has been demonstrated to be able to detect one abnormal cell in a sea of hundreds of thousands of similarly appearing and overlapping normal cells. It is this advance in computer science that makes the OralCDx test so extremely sensitive and reliable.
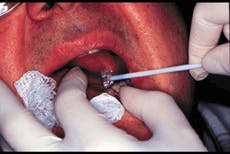
Use of the biopsy brush
Another important advance was providing the dentist with an easy-to-use biopsy brush (Figure 1) that can get down to the basal cells. This makes the oral-brush biopsy very unlike the exfoiliative cytological smears, such as traditional oral-cytology smears or cervical pap smears. Both of the latter exams only pick up superficial cells. By getting to the basal cells, the dentist can pick up cells that are more pathognomonic of this dysplastic change.
What I am discussing was the foundation of an extensive article in the October 1999 issue of JADA. For those who may have missed that article, a pipebrush-like device is pressed against an area of the mucosa that is red, ulcerated, or for some other reason appears suspi-cious (Figure 2). With half a dozen turns, the brush will pick up basal cells. The experience is sometimes a little irritating to the patient`s tissue, but it certainly does not necessitate a local or topical anesthetic and obviously no scalpel biopsy is needed.
The tissue removed is then spread onto a glass slide and a fixative is added. It is allowed to dry before being sent off to the OralScan laboratories (Figure 3).
At the lab, pathologists examine the slide, aided by the neural network computer (Figure 4). The dentist recieves a report back from the lab, indicating its findings - i.e., whether there is a positive, atypical, or negative finding. The results show an amazing degree of accuracy.
What to say to patients
For most of us, the challenge is communicating our concern about a lesion that does not seem sufficiently large or sinister enough for us to recommend a scalpel biopsy. It may be the sort of finding that a hygienist has made in the course of his or her scrutiny of the oral tissues. The exchange with the patient that works the best for me goes something like this:
"Mrs. Jones, I see something on the side of your tongue which is probably benign and nothing to be concerned about. But, it is always best to make sure because of the small chance it may not be benign and I`m certainly not infallible. If it turns out not to be benign, the good news is that it`s usally completely curable in a pretty straightforward procedure if it is detected early. We have a test that I can do which is quite painless. It will allow us to know for sure if this lesion is of no concern."
In most cases, the report faxed back from the lab will be negative and then the patient can be reassured. An important safeguard with OralCDx is that the dentist`s procedure is "fail safe." This means that in the event that the dentist failed to get down to the basal cells - which is not likely, but can occur, because there is always a learning curve with everything - this is automatically detected by the computer and pathologists at OralScan. The test is then repeated at no charge.
High cost of treatment
Economically, this is a very important development. Some 30,000 oral cancers are diagnosed every year in the United States. My inquiries indicate the usual cost of treating an oral cancer case in the Midwest would be between $80,000 and $90,000 - apart from the fact that the patient is going to lose a year or two of his or her life! The survival rate after five years is about 50 percent. It`s pretty obvious that the earlier it is detected, the better the chance of resection and removal.
At the same time, we have to recognize that a dentist often will see an aberrant area and only make a mental note to "keep an eye on it." Or, if the patient is a smoker, the dentist will try to impress upon him or her the need to quit smoking. How much stronger that advice would be if, after a brush biopsy, you could inform the patient that the test showed dysplasic changes. That`s a bit better than saying to the patient, "I`m going to keep an eye on it," or "Do you think it`s changed much?"
Several studies have shown that, in the course of a week, the general dentist will see two to six patients with some type of oral lesions. Many of these are very subtle mucosal changes, such as flat, tiny, white or red areas. Since these lesions are so common and the vast majority of them are benign, most were only watched or ignored in the past when the only tool available to test them was the scalpel biopsy. As a result, only those lesions with the highest degree of clinical suspicion were ever tested, leaving many precancerous lesions to go undiagnosed and thus allowed to progress. Unfortunately, lesions with a high degree of clinical suspicion often represent late-stage disease. Of course, the prevalence of oral lesions in a particular practice will depend upon the average patient age and the proportion of patients who use tobacco.
Proof of the pudding is, as they say, in the eating. In a large series, the OralScan system found every case of histologically confirmed precancer and cancer; it was extraordinarily reliable. Further-more, when the analysis was completed on lesions which were not clinically suspected of being harmful, OralScan picked up a number of precancers and cancers proven by subsequent scalpel biopsy.
Introductory kit
The kits containing the testing material (Figure 5) always are provided to the dentist at no charge. In the introductory package, a free instructional video also is provided that is very informative. It fully demonstrates the technique to be used in this procedure.
You start with five introductory test kits that are supplied at no charge. As you use them, the company will replace them at no charge. If payment for the laboratory-analysis fee of $65 is not enclosed with the test, the company bills the patient`s insurance for it. Insurance usually does reimburse both the dentist for performing the procedure (about $100) and the laboratory for the reading of the biopsy (approximately $65). ADA and CPT codes which the dentist can use to bill for the biopsy procedure are provided with the test kits. However, patients generally are very thankful to the dentist for providing this potentially lifesaving clinical service, and they usually are more than willing to pay for the test if oral biopsies are not a covered benefit of their dental plans.
To me, this technology can enhance not only the thoroughness of the oral exam, but also the practitioner`s diagnostic skills and clinical acumen. When you examine either a new patient or a patient-of-record at a recall visit, areas that previously were put "on a long finger" (to keep an eye on because they did not ignite your index of suspicion) can now be brush-biopsied in minutes. Areas that a patient has noticed - though patients don`t usually notice them unless there is soreness involved - can be brush-biopsied at a moment`s notice.
I recall reading that once a change has affected about 30 percent of the population, that change then has reached what is called "critical mass" and the further promulgation of the technique or process is very rapid. We have seen that process occur in many areas of our lives - with the use of personal computers in our homes, e-mail, the Internet, and cell phones, just to name a few. The use of this new technology started slowly with just a few people. Then, suddenly, it gathered momentum with the speed of a snowball rolling down a mountain. If you found yourself not using this new technology, you were suddenly "out of the loop."
Computers are now a part of most dental practices. Initially, they were used for appointments, billing, and monitoring supplies. Now, we use them in the operatory to do digital radiography and even laser restorations. Computerization has even become part of the oral exam and diagnosis process.
The same thing can happen with oral-cancer detection. By using the new tools available to us, we can create a new health trend with the potential to save many lives. All it takes is for you to do your part in making use of this new technology.
Editor`s Note: Neither Dr. Leonard nor the clinic in which he works received any tangible or intangible benefits for using the instruments or techniques named in this article.
For more information on OralScan and sample kits, call (800) 560-4467 or visit the company`s Web site at oralcdx.com.
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5