Dr. Joe Blaes conducts a rare one-on-one interview with Dr. Joe Massad
For more on this topic, go to www.dentaleconomics.com and search using the following key words: removable dental prosthetics, fixed dental prosthetics, TMJ health, dentures.
Q: Why don't more clinicians embrace removable prosthetics?A: First, I would emphasize the need to update the dentist's skills so that he or she is ready to deliver today's state-of-the-art prosthesis. Second, it is extremely vital that all of the armamentarium be available and the staff be fully trained on the proper utilization of each instrument. Third, each dentist must determine his or her policies with a very detailed informed consent that explains in simplified terms what each patient should expect. Finally, and possibly the most important, it is crucial to secure a well-trained laboratory to handle all removable procedures. The prosthetic lab technician is the vital thread to sew up cases with predictability. Q: How can removable prosthetics be a profit center in a dental office?
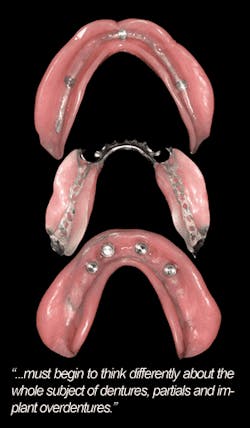
When patients maintain dentures or partials for 20 plus years, we often see conditions such as severe bone atrophy, premature tissue character loss from fibrous to fragile, and increased tissue mobility. These degenerative processes can be slowed down significantly by maintaining a proper fitting prosthesis. In actuality, dentistry has a shelf life that we should make our patients aware of. As the body ages, we must intervene to give patients the best quality of life available.
Here are the protocols I suggest for my patients. I will start with complete dentures. Patients are asked to return every six months for a tissue check and denture fit evaluation. At the one-year recall, patients are evaluated for both fit and occlusion. Some patients may need minor occlusal adjustments and some may need relining. If, for example, resilient liners are placed at delivery, there is a good chance the severely resorptive patient will need a replacement liner. On average, soft liner should be replaced every one to two years depending on the overall condition and health of the patient.
Next, I will talk about implant overdentures. Since two to four implant abutments are average, we still have tissue load and indications of relining from time to time. If a ball ring, nylon female attachment or soft liner is used for the retention, then each of these will lose its resiliency and need to be replaced. Replacement is generally attributed to hygiene, occlusal load, dry mouth, and some medications that create unfavorable mouth environments. On average, attachment retentive elements should be replaced every one to three years for optimal performance.
Finally, I'll discuss partial denture prostheses. Depending on the number of remaining teeth, relining the edentulous area should be treated like complete dentures. If the patient does not seem to have loose partial dentures, it does not necessarily mean the fit is optimal. Total replacement of cast metal frame on conventional partials should occur every five to 10 years. There are, however, many more factors due to the presence of dentition. From a health perspective, we are helping our patients. From a financial perspective, we are increasing the billable procedures and are thus building a profit center rather than a depression center.
References available upon request.