Ask Dr. Christensen
by Gordon J. Christensen, DDS, MSD, PhD
For more on this topic, go to www.dentaleconomics.com and search using the following key words: small-diameter implants, conventional-diameter implants, dentures, ridge calipers, hands-on courses.
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics® readers. If you would like to submit a question to Dr. Christensen, please send an e-mail to [email protected].
Q I am impressed with the reported success of small-diameter implants used to support and assist in retaining complete dentures. Are these narrow-body implants going to replace wider-diameter implants? Are they less expensive for patients than wide-body implants? If not, what are the advantages as you see them related to the use of small-diameter implants versus standard-diameter implants?A After placing and restoring root-form dental implants for several decades, your question is especially pertinent to me. I am at a turning point in my career, as I see these small-diameter implants (SDIs) serving well, and I often have to make a decision about whether to use conventional-diameter implants or small-diameter implants in situations in which I used only conventional root-form implants in the past. To answer your question, I will discuss the apparent advantages of small-diameter implants as long-term treatment.CLINICIANS REPORT (formerly the CRA Newsletter) surveyed 200 users of SDI. The survey was very positive, reporting 91% survival. The details of that survey will soon be published in The Journal of Restorative and Esthetic Dentistry. I have written several articles reporting my views on small-diameter implants and conventional-diameter implants. Additionally, several other papers support the usefulness of SDIs. In the survey, the main use of SDI was reported to be in edentulous arches, which directly relates to your question.
I will provide an answer to your question by comparing the techniques for conventional diameter (3 mm and over) and SDIs (<3 mm diameter) for stabilization and retention of mandibular or maxillary complete dentures. I will compare the steps in the techniques from the standpoints of the patient and the dentist and his or her staff.
• Diagnostic needs. Both SDIs and conventional root-form implants require similar diagnostic activity, including a detailed health history, dental history, and other standard diagnostic procedures. However, the need for more radiographs is evident.
Some practitioners place either type of implant without facial-lingual orientation radiographs which show the quantity and quality of bone. I suggest that radiographs showing the quantity and quality of bone in a facial-lingual orientation should be used for both SDIs and conventional-diameter implants. Such radiographs assist in predicting the ability of the bone to support SDIs.
If the bone is highly trabeculated (porous) in a facial-lingual dimension, SDIs are not indicated. If the bone has dense cortical bone on the facial and lingual aspects of the maxilla or mandible — and lack of density in the center portion — SDIs are usually not indicated. Standard panoramic radiographs cannot demonstrate the needed information. If practitioners use panoramic radiographs only, they may find that the SDIs do not have adequate bone support and they will fail. In my opinion, panoramic radiographs, occasionally periapical radiographs, and some type of facial-lingual radiographs (tomographic, CT scan, or cone beam) are necessary for adequate diagnosis for implants, treatment planning, and surgical placement.
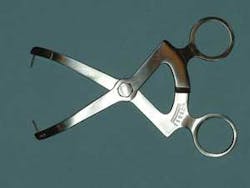
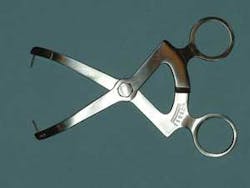
Are measuring devices showing the amount of bone present in a facial-lingual dimension to be acceptable? Ridge measurements in a facial-lingual dimension — made by a ridge caliper — provide guidance about the quantity of bone present, but do not provide observation of the density of bone. Salvin® Dental Specialties has such a device available (Figure 1). Ridge calipers provide a good diagnostic estimation of bone present prior to obtaining acceptable radiographs.
When placing only a few implants, I prefer to use individual, specific-location tomographic radiographs of the proposed implant sites to show the facial-lingual quantity and quality of bone. Such radiographs are desirable even if you are not planning to accomplish the surgery yourself. In my practice, we are currently using a Planmeca panoramic device with a tomographic option (Figure 2). Of course, conventional CAT scans can be used if available in your area. In summary, the collection of diagnostic data is relatively simple and about the same for both SDI- and conventional-diameter implants.
• Placement of the implants. Conventional implants are placed with or without a surgical flap procedure, depending on the amount of bone present and the desires of the person performing the surgery. Making a flap is a simple procedure, but it is more traumatic for patients than placing the root-form implant through the soft tissue without a flap. Clinical research has shown a slight resorption of bone when a flap is made.
In general, most conventional-diameter implants are placed using the following technique: making a flap, placing the implant, suturing the flap, waiting for a few months for osseointegration to occur, and loading the implants. Clinical studies meticulously assembled into meta analyses have not provided conclusive data about whether or not immediate loading is good or bad. There are positive and negative data on both sides of the question.
I load conventional diameter implants if, when initially placed, they appear to be solidly stabilized in dense bone. If there is any question in my mind about the bone quality, I prefer to wait a few months (four months for the mandible and six months for the maxilla) before loading the implants. I have experienced fewer failures than the international data show when using this cautious approach.
For example, let's use a complete denture as an example case. Two implants are the minimum number of conventional-diameter implants I feel comfortable with when implants are planned to provide support and retention for complete dentures. One implant is placed in each canine area. I then prefer to wait four to six months for osseointegration before loading the implants. During this wait time, the implants remain either submerged under the soft tissue or with healing caps on them with soft denture liner in "wells" that have been cut in the denture base in the location of the implants.
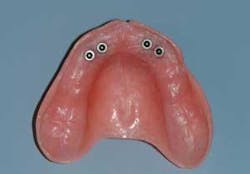
When placing SDIs, the situation is very different. In the CLINICIANS REPORT survey, 80 percent of SDIs were placed without a flap. I agree with the conclusions of the survey respondents. I suggest that four SDIs should be placed in each edentulous arch, two in each canine area. (Figures 3 and 4). These implants should vary from 1.8 mm in diameter to nearly 3.0 mm in diameter. Most SDIs appear to be similar to a wood screw (Figure 5). The initial osteotomy in the bone is made only a few millimeters deep. The screw cuts its own deeper osteotomy by extending several additional millimeters into bone, widening the bone as it is screwed in. The most commonly used length of SDIs is about 13 mm. Since the original osteotomy is not made to the final depth of the SDI, the SDI angle of direction can be changed as it is screwed into bone to align it into the necessary path of insertion with other implants.
This surgical procedure is relatively atraumatic when a flap is not made. Usually, two SDIs are placed where only one conventional implant would have been used. They must be placed a few millimeters apart to allow placement of housing for each SDI into the denture. Using two SDIs ensures that there is an equivalent amount of implant-to-tooth interface when compared to one conventional-diameter implant. Placing four SDIs under the denture also ensures that the SDIs cannot be rotated when they are loaded (before they have achieved osseointegration).
• Loading the implants. SDIs are almost always loaded on the day of placement — or a day or two later — to allow adequate time for laboratory work. Conventional-diameter implants are usually loaded months later when used as single implants not connected to other implants. The patient benefits from the SDIs almost immediately:
• Cost of small-diameter and conventional-diameter implants for edentulous patients. Although SDIs are significantly less expensive purchased from manufacturers than most conventional-diameter implants, more SDIs are used per patient, making the total cost relatively comparable. The overall cost to patients for either service is about the same.
According to our survey1, the average cost for placement of one conventional-diameter implant was $1,542 for the 200 dentists in this survey. The cost of placing SDIs was $650 per implant. Therefore, the cost of two conventional-diameter implants was about $3,084, while four SDIs cost about $2,600. An average U.S. fee for one denture is approximately $1,200, making the overall total cost using two conventional implants and an overdenture about $4,284, and an overdenture supported by four SDIs about $3,800. Of course, your fees may vary widely from those reported in the survey. Cost differences do not appear to favor one technique or the other.
• Service potential of small and conventional implants in edentulous situations. After several decades of placing two conventional-diameter implants under complete dentures, and eight years placing four SDIs under complete dentures, I have concluded that patient satisfaction and service potential for the two concepts are the same for edentulous situations.
• Patient advantages. The advantages of the SDI concept for patients are very clear:
- Less trauma. Usually SDIs are far less traumatic to place than conventional-diameter implants used with a flap procedure.
- Faster procedure. The SDIs can be placed in a few minutes by an experienced clinician, much faster than the procedure for placement of conventional implants.
- Immediate loading. Implant loading can be immediate without a flap or within a few days if a flap was made.
- May be less expensive. Although some conventional implant techniques can be far more expensive than the SDI concept, the two techniques can be close in cost.
• Dentist advantages. Dentists placing conventional diameter implants find that the following advantages are soon evident with the SDI concept:
- Easier to align implants and overall easier procedure. The self-tapping nature of the screw-form SDIs allows alignment with other implants and the path of insertion while actually placing the implants is much easier than its conventional implant counterpart.
- Can be placed in minimal bone. The osteotomies made for SDIs are small, narrow, and only a few millimeters deep. The bone surrounding the implants and apical to the implants is expanded by the screw effect of the implants. Therefore, bone 4 mm from facial to lingual is expanded by screwing the SDIs into the bone to at least 6 mm. In the case of conventional-diameter implants, the osteotomy is only slightly smaller than the size and depth of the implant, requiring more bone to be present.
- Immediate loading is the standard technique. Loading of implants on the day of implant placement or the next day allows laboratory time, facilitates completion of the procedure, and enhances patient acceptance.
- No flap. A flap is usually not needed (80% of the time).
- Fast healing if implant fails. If SDIs fail in service, they are easily removed. When removed, the bone fills radiographically over about a two-week period, compared to months required for bone to fill a space where a conventional implant was removed.
This has been a long answer to your question. I feel that many patients who need support and enhanced retention of complete dentures are not receiving them because of their fear of the surgery, lack of knowledge about where implant care can be obtained, and in many cases, high cost. The relatively atraumatic SDI concept can provide significant service to a wide population of edentulous patients. I encourage any surgically-oriented dentists, regardless of their education or specialty, to examine the SDI concept.
The answer to your question is yes, small-diameter implants, properly placed in appropriate patients, are offering superb, immediate, and relatively moderate-cost solutions to oral challenges due to edentulism. They do compete well with conventional-implant techniques.
Hands-on courses available
Implant surgery and implant restoration are subjects of great interest in the profession. We offer conventional–diameter ("Simplified Implant Surgery") and mini&ndah;implant ("Mini Implants, Easy Placement and Immediate Restoration") hands-on courses at the Scottsdale Center for Dentistry.
These courses are among our most in-demand subjects. For more information on these small-attendance, hands-on courses, contact Practical Clinical Courses at (800) 223-6569 or visit our Web site at www.pccdental.com.
Dr. Christensen is a practicing prosthodontist in Provo, Utah, and Dean of the Scottsdale Center for Dentistry. He is the founder and director of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Rella) and senior consultant of CLINICIANS REPORT (formerly Clinical Research Associates), which since 1976 has conducted research in all areas of dentistry.