Guided biofilm therapy is and remains the absolute favorite
People who wish to stay healthy also attach importance to their oral health and regularly go for professional prevention. Following treatment with guided biofilm therapy (GBT), over 278,000 patients worldwide were surveyed using standardized questionnaires. Of these, 94% prefer GBT to conventional methods and therefore recommend it to family and friends. Patients were also asked about their perception of pain, the time required, and the meaningfulness of disclosing.
Due to the high burden of disease, the World Health Organization (WHO) has declared oral diseases—including caries and periodontitis—as a key health problem.1,2 To get this under control, and in addition to a healthy lifestyle, microbial plaque (biofilm) must be removed regularly and completely. However, daily personal oral hygiene removes a maximum of 50% of the biofilm from supragingival tooth surfaces, particularly in the interdental region.3
As a second cornerstone, regular and effective professional prevention is crucial.4,5 For this to be successful, it must be patient-friendly and reflect current knowledge and technical progress.6-11 In response to these requirements, EMS Dental developed the concept of guided biofilm therapy in collaboration with leading experts.12 To determine the acceptance of GBT compared to conventional methods, patients of GBT-certified practices were surveyed using standardized questionnaires.
Methods and results
Part of the certification protocol includes GBT training of the entire practice team by the Swiss Dental Academy (SDA) and obtaining patient feedback. The anonymized responses (n = 278,258) were provided to EMS by 13,082 GBT-certified practices (as of October 31, 2023).
The questionnaire used for feedback comprises of seven questions to be rated on a scale of 0 to 5. All demonstrated a very high level of acceptance for GBT with approximately 4.7 out of a possible 5.0 points. Patients also rated the appropriate amount of time required and the absence of pain. With a percentage of 93.93%, they clearly preferred GBT to the conventional method (figure 1). 93.17% of respondents considered disclosing to be meaningful. This step in the GBT protocol ensures that biofilm has been removed completely, which is quality assurance for the patient and practitioner. The University of Zurich was involved in the further development of the questionnaire.
Discussion
In conventional teeth cleaning, hard deposits are first removed using invasive sonic, ultrasonic, and hand instruments.13 Subsequent polishing also results in the loss of valuable tooth substance without achieving a better surface smoothness.14 In addition, disclosing is often not performed.15 By contrast, GBT first removes the biofilm which is the etiologic factor from all oral surfaces. This is performed—after obligatory disclosing—in a minimally invasive and gentle manner with Air-flowing (figure 2).16
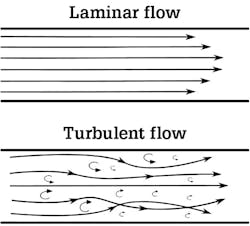
Highest effectiveness and efficiency are demonstrated by the Airflow Prophylaxis Master with the Airflow Max thanks to the patented Laminar technology, Perioflow and Plus Powder (figure 3).17 In case of any visible remaining hard calculus, the piezoceramic ultrasonic system (Piezon PS No Pain) is used.
Present-day well-informed patients desire prevention management that is both effective and state-of-the-art, delivered in collaboration with the dental team on a personal level. The lack of discomfort and the positive encounter with gentle preventive care are crucial factors for fostering patient loyalty in terms of recall, and consequently, they significantly contribute to the economic success of a dental practice.
GBT has also been shown to be superior in these aspects, both in primary (PMPR) as well as in secondary and tertiary supportive periodontal therapy (SPT).6,7,9-11
Conclusion
In summary, more than 278,000 patient surveys unequivocally affirm the widespread acceptance of the GBT protocol. This endorsement was previously substantiated in an evaluation from April 2022 (https://gbt-dental.com/US-278k-GBTPS-1).18 While the enthusiasm of the prevention team for GBT might influence patient evaluations (Hawthorne effect),19 the survey results align closely with findings from published studies in both dental practices and academia.20 Given the diverse research inquiries and the substantial participant pool, a distinct preference for GBT over conventional methods can thus be confidently established.
Editor’s note: First published in ZMK, Jg. 39, Ausgabe 11-12, November/Dezember 2023. 634-645, Spitta GmbH. Reprinted with permission. This article also appeared in the February 2024 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Blas E, Kurup Introduction and methods of work. In: World Health Organization: Equity, social determinants and public health programmes. World Health Organization; 2010:3-10.
- World Health Organization. Political declaration of the third high-level meeting of the General Assembly on the prevention and control of noncommunicable Report by the Director-General. Executive Board EB150/7, 150th session. January 11, 2022, Provisional agenda item 7. 2022.
- Sälzer S, Graetz C, Dörfer CE, Slot DE, Van der Weijden FA. Contemporary practices for mechanical oral hygiene to prevent periodontal disease. Periodontology 2000. 2020;84(1):35-44. doi:10.1111/prd.12332
- Axelsson P, Nyström B, Lindhe The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J Clin Periodontol. 2004;31(9):749-757. doi:10.1111/j.1600-051X.2004.00563.x
- Tonetti MS, Chapple ILC, Jepsen S, Sanz M. Primary and secondary prevention of periodontal and peri-implant diseases: introduction to, and objectives of the 11th European Workshop on Periodontology consensus conference. J Clin Periodontol. 2015;42(Suppl 16):S1-S4. doi:10.1111/jcpe.12382
- Bastendorf K, Strafela-Bastendorf N. Auf das klinische Protokoll kommt es an – PZR, UPT und Quintessenz. 2020;71(12):1380-1389.
- Vouros I, Antonoglou GN, Anoixiadou S, Kalfas S. A novel biofilm removal approach (Guided Biofilm Therapy) utilizing erythritol air-polishing and ultrasonic piezo instrumentation: a randomized controlled trial. Int J Dent Hyg. 2022;20(2):381-390. doi:10.1111/idh.12533
- Bischoff Herausforderung Prophylaxezentrum. Zahnarzt Wirtschaft Praxis. 2018;(6):16-19.
- Bühler J, Amato M, Weiger R, Walter C. A systematic review on the patient perception of periodontal treatment using air polishing devices. Int J Dent Hyg. 2016;14(1):4-14. doi:10.1111/idh.12119
- Bühler J, Amato M, Weiger R, Walter C. A systematic review on the effects of air polishing devices on oral Int J Dent Hyg. 2016;14(1):15-28. doi:10.1111/idh.12120
- Fu JH, Wong LB, Tong HJ, Sim YF. Conventional versus comprehensive dental prophylaxis: comparing the clinical outcomes between rubber cup and air polishing and the importance of plaque disclosure. Quintessence Int. 2021;52(3):264-274. doi:10.3290/j.qi.a45602
- Lang N, Lussi A. Bastendorf Scientific consensus guided biofilm therapy protocol. A new concept to primary and secondary prevention. E.M.S. Electro Medical Systems. 2019. https://gbt-dental.com/ZMK1112-23-SP-ENG-Consensus
- Arefnia B, Koller M, Wimmer G, Lussi A, Haas M. In vitro study of surface changes induced on enamel and cementum by different scaling and polishing. Oral Health Prev Dent. 2021;19(1):85-92. doi:10.3290/j.ohpd.b927695
- Burkhardt AS, et al. Effect of air-polishing using erythritol on surface roughness of enamel and dentine compared to conventional methods. Poster presented at the EuroPerio, Copenhagen. 2022.
- Stiftung Warentest. Weit aufmachen, Stiftung Warentest: Professionelle Zahnreinigung. 2015;(7):86-90.
- Mensi M, Scotti E, Sordillo A, Agosti R, Calza S. Plaque disclosing agent as a guide for professional biofilm removal: a randomized controlled clinical trial. Int J Dent Hyg. 2020;18(3):285-294. doi:10.1111/idh.12442
- Donnet M, Fournier M, Schmidlin PR, Lussi A. A novel method to measure the powder consumption of dental air-polishing devices. Appl Sci. 2021;11(3):1101. doi:10.3390/app11031101
- Koch “Guided Biofilm Therapy“ is the absolute favorite among patients. Worldwide survey on the preferred method of oral prevention. ZMK. 2022;38(4):183-185. https://gbt-dental.com/ZMK1112-23-SP-ENG-OralHealth
- Feil PH, Grauer JS, Gadbury-Amyot CC, Kula K, McCunniff MD. Intentional use of the Hawthorne effect to improve oral hygiene compliance in orthodontic patients. J Dent Educ. 2002;66(10):1129-1135.
- Furrer C, Bättig R, Votta I, Bastendorf KD, Schmidlin PR. Patient acceptance after of «Guided Biofilm Therapy». Swiss Dent J. 2021;131(3):229-234. https://gbt-dental.com/ZMK112-23-SP-ENG-Furrer-C
Dr. med. dent. Jan Hermann Koch is a licensed dentist with several years of practical experience, located in Freising, Germany, focusing on conservative dentistry, pediatric dentistry, and periodontology. He has more than 20 years of experience as an editor, independent journalist, and public relations professional. He received his dental degree from the University of Berlin and is a member of the Bavarian Dental Association and the German Association of Oral and Maxillofacial Medicine.
About the Author

Dr. med. dent. Jan Hermann Koch
Dr. med. dent. Jan Hermann Koch is a practicing dentist in Freising, Germany, focusing on conservative dentistry, pediatric dentistry, and periodontology. He has more than 20 years of experience as an editor, independent journalist, and public relations professional. He received his dental degree from the University of Berlin and is a member of the Bavarian Dental Association and the German Association of Oral and Maxillofacial Medicine.
Updated January 25, 2024