As the prevalence of implants grows as a popular choice to replace natural teeth, so do their problems. Implant failure is on the rise, and the number one reason for that is peri-implantitis, which is caused by excessive biofilm. The only way to remove this biofilm is to help patients create an easy at-home regimen. The problem is that implants are often placed into the mouths of patients who more than likely lost their natural tooth (or teeth) due to poor oral hygiene for years. Similar to most oral issues, implant failure begins with poor home care. Although the tooth has now been replaced, the problem still remains. Helping patients understand that implant failure happens for the same reasons their natural tooth failed is critical to long-term implant success. As dental professionals, we need to equip patients with the right tools and information the moment they become a candidate for implant placement. Let’s investigate methods that help to manage implants and the onset of peri-implant disease.
Before the implant is placed
Patients who lost their natural teeth due to poor oral hygiene need to understand that without reform, the same problem will likely persist. We could apply the logic that many orthodontic practices use prior to treatment—the patient has to “prove” that they are able to keep their teeth clean. If not, treatment is delayed until they are able to show improvement. Similar to orthodontics, patient compliance determines the success of an implant. Implants pose a particular challenge from the beginning since we are asking those who have poor oral hygiene not to brush or floss the surgical site for several weeks while it heals. This simply reinforces the bad habits that were already in place.
Related reading:
- Dental implant maintenance to reduce peri-implantitis risk
- Dental implants versus fixed prostheses
- Is an implant better than a tooth?
To ensure long-term success of an implant and prevention of peri-implantitis, one of the most important tasks for a patient is the management of biofilm (dental plaque). Several studies report that biofilm is the key etiological factor in the development and progression of peri-implant infections.1,2 Products such as toothpaste, floss, water irrigators, interdental brushes, etc. provide mechanical means of removal; they don’t have the therapeutic abilities of being able to break up biofilm or kill bacteria (and other pathogens). Around an implant specifically, biofilm can be hard to remove because it is hard to access with normal brushing and flossing. So something with therapeutic benefits and the ability to access hard-to-reach areas must be used.
Maintaining implant health
There are a number of clinical interventions to aid in the treatment of peri-implant diseases, but prevention and early detection of issues are key to successful outcomes.3 Overall poor health, poor dental health, and infection are all reasons implants can fail in the early stages of placement. Therefore, maintaining healthy hard and soft tissues surrounding the implant is critical, because the tissues act as biological barriers in preventing peri-implant disease.1
The microorganisms linked to peri-implant disease are quite similar to those that cause periodontitis.4 These include bacteria, viruses, fungi, volatile sulfur compounds, and biofilm. Just like in periodontal disease, the pathogens become more complex as they mature and are left behind in uncleaned, undisrupted areas of the mouth. This makes them harder to remove with time, resulting in peri-mucositis, the initial infection that presents around a poorly cared-for implant. This can be reversed as opposed to more aggressive, irreversible peri-implantitis. As dental professionals, it is our job to help prevent the onset of this disease and guide patients in the tools that they need to achieve the best results.
Reducing the risk for implant failure
So how can we help? Protection for implants needs to begin during the healing process. Ideally the protection would begin during surgery, using therapeutic agents to help reduce contaminants in the surgical site. Then patients should continue to keep the area clean using a rinse, since they can’t use mechanical means of disruption during this phase. This will not only create a more ideal environment for healing, but will also reinforce the need for the specialized care of their newest addition. A rinse could aid in providing long-term maintenance for the implant.
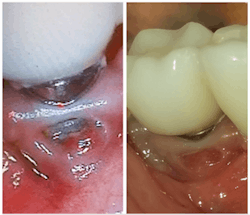
We educate our patients on brushing and flossing and hope they do this on a regular basis, but even when they do brush and floss, it is still only mechanical. IfStudies have concluded that therapeutic substances in certain products are able to reduce the viability of pathogens in biofilm.6-10 Activated chlorine dioxide is such a substance. It has the ability to kill bacteria, viruses, and fungi, break up biofilm, and reduce volatile sulfur compounds. This active ingredient can be safely used daily for both implant and regular hygiene (figure 1). One such product that contains these ingredients is OraCare’s Reassure system. This product has a gel to help immediately during surgery, and a rinse to help the patient at home.
With the growing popularity of implants, it is up to us to find better ways to keep peri-implantitis at bay. Since we know that implants mostly fail due to poor home care, we must provide patients with the proper tools. Creating a daily regimen that includes a rinse with therapeutic benefit is our best defense against the number one cause of implant failure.
Editor's note: This article appeared in the November 2021 print edition of Dental Economics.
References
1. Prathapachandran J, Suresh N. Management of peri-implantitis. Dent Res J (Isfahan). 2012;9(5):516-521.
2. Pedrazzi V, Escobar EC, Cortelli JR, et al. Antimicrobial mouthrinse use as an adjunct method in peri-implant biofilm control. Braz Oral Res. 2014;28(1):1-9.
3. Smeets R, Henningsen A, Jung O, et al. Definition, etiology, prevention and treatment of peri-implantitis–a review. Head Face Med. 2014;10:34.
4. Heydenrijk K, Meijer JA, Van der Reijden WA, et al. Microbiota around root-form endosseous implants: a review of the literature. Int J Oral Maxillofac Implants. 2002;17:829-838.
5. Eke PI, Dye BA, Wei L, et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91(10):914-920. doi:10.1177/0022034512457373
6. Felo A, Shibly O, Ciancio SG, et al. Effects of subgingival chlorhexidine irrigation on peri-implant maintenance. Am J Dent. 1997;10(2):107-110.
7. Ciancio SG, Lauciello F, Shibly O, et al. The effect of an antiseptic mouthrinse on implant maintenance: plaque and peri-implant gingival tissues. J Periodontol. 1995;66(11):962-965.
8. Gosau M, Hahnel S, Schwarz F, et al. Effect of six different peri-implantitis disinfection methods on in vivo human oral biofilm. Clin Oral Implants Res. 2010;21(8):866-872.
9. Baffone W, Sorgente G, Campana R, et al. Comparative effect of chlorhexidine and some mouthrinses on bacterial biofilm formation on titanium surface. Curr Microbiol. 2011;62(2):445-451.
10. The science behind OraCare scientific studies and research. OraCare. Accessed September 1, 2021. https://www.oracareproducts.com/studies--scientific-research.html
About the Author

Robert Martino, DDS
Robert Martino, DDS, is a 1990 West Virginia University School of Dentistry graduate. Currently, Dr. Martino owns and operates seven dental practices in West Virginia, presiding as CEO of Wilmar Management Company. Dr. Martino is also a founder and CEO of EASW, a worldwide aeronautics company focused on repairing airplanes and their engines. In 2013, Dr. Martino founded Freedom Day USA, a national thank you movement for active military, veterans, and their immediate family members.
Updated October 11, 2021