Wake the sleeping giant in your practice
by Dr. Brad Guyton, Dr. Steve Poss, and Misty Clark
Some of our clients contacted us recently and had questions about integrating a sleep therapy component into their practices. In this article we've tried to address some of their top questions and concerns.
- What is OSA?
- Aren't CPAPs the treatment of choice?
- Do you have step-by-step recommendations on how to get started?
Guyton: First, we all need to know that obstructive sleep apnea (OSA) is when your patient stops breathing for more than 10 seconds at a time, due to some form of obstruction. Dental treatment of obstructive sleep apnea may be a viable option for some patients. There are typically three treatment options for the OSA patient: 1. Surgical correction of obstructions, 2. Use of a CPAP device, and 3. An oral appliance (often effective for mild to moderate OSA). For nonsurgical candidates, the CPAP is still the gold standard for patients with severe OSA. While severe OSA is characterized by breath cessation for more than 10 seconds at least 30 times in one hour; for patients with these cessation events occurring less than 30 times per hour or for patients who refuse a CPAP device, an oral appliance may often be an appropriate treatment option. As dentists, we can screen our patients for this condition.
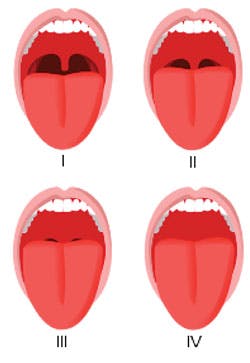
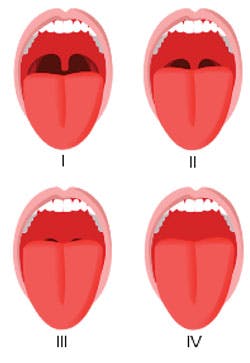
Poss: Absolutely. Since we have the opportunity to evaluate our patients twice a year, we have included the Epworth Sleepiness Scale in our patient health update. We ask how tired our patients are, if they feel refreshed after sleeping, and if they have ever been diagnosed with sleep apnea. If they have a CPAP, we determine if they are using it as prescribed. We know that half of the patients prescribed with CPAPs stop using them within the first two years. We incorporate the Mallampati classification of the soft palate into our screening process (Figure 1).
Source: Wikipedia
Guyton:: For dentists to successfully integrate dental sleep medicine to their practices, it is imperative to develop a relationship with a sleep medicine physician. As dentists, we cannot diagnose sleep apnea.Poss:: Because of this, we refer our at-risk patients to their primary care physician or a sleep physician. If the patient has had a sleep study (PSG) in the last five years, we may request a copy of the PSG and a prescription from the physician for the fabrication of an appliance. In cases when the patient is not convinced that they may have a sleep breathing disorder, then we can screen the patient with a home sleep testing monitor (HST) such as Ares by Watermark or SleepView by CleveMed. At that time, the patient can be directed to the sleep clinic for a full PSG and a resulting complete diagnosis. This partnership with the physician is the approach we recommend as OSA has the potential for very serious health consequences.Guyton:: We know that approximately 100 million Americans snore, and that roughly a third of them are expected to have some form of sleep apnea. Sadly, only 3 million of these patients are estimated to have been diagnosed to date. That means almost 90% of your patients might be undiagnosed. It is time to get the word out to our patients.
Clark: There are some major things to consider when getting the word out. Simply adding the treatment of OSA to your mix will not mean that patients will be leaping out of the chair to have it. First, they need to know that you are now offering a service to treat sleep apnea. Your second challenge is that there is an education gap in the general population -- people don't know they have it. If you want to treat sleep apnea, then your patients need to know that they could be a candidate. What we know is that people need to hear, see, feel, and/or experience a message five to seven times before acting on it. Make sure you have an internal marketing strategy in place to educate your patients about what sleep apnea is, what symptoms to look for, and that you can help them. You must plan and execute if you want to be effective!
Guyton:: Once you have mined your existing patients, you need then to think of this as a different business within your practice. External marketing then becomes paramount.
Clark: OSA treatment is a marketable service that draws attention to your practice and can bring in new patients. Remember, be confident in your message, repeat it often, be action oriented, and include an enticing offer. Consider visiting with the local sleep physicians and hosting a lunch-and-learn. Let them know you are available to assist with the mild to moderate CPAP-intolerant patients. As with any new service in your practice, you need a strategic marketing plan in order for you to be effective.Poss:: In addition to the marketing plan, you need an effective process once the patients are in the office. You must develop a robust referral network. Every dental office has plenty of CPAP-intolerant patients. Most often, these patients already know and trust you. Screen every adult patient in your office. For patients with suspected OSA, invite their sleeping partner to come to the visit so that they might confirm the snoring, breathing cessation, and or gasping during sleep. Know what risk factors to look for and be well educated so that you can answer your patients' questions.Guyton:: Some of the common risk factors are: 1. Obesity (BMI>30), 2. Snoring, 3. Neck circumference > 17 inches for males or >16 for females, 4. Gastric reflux, 5. High blood pressurePoss:: Once you identify your patient's risk profile as part of your initial screening, consider these next steps:
- Visit 1: Consultation to discuss the symptoms and risk factors. Include a complete head-and-neck exam including muscles and TMJ.
- Discuss financial arrangements and medical insurance.
- Schedule an appointment for the patient with your local sleep lab or their primary care physician. Send a letter with your findings to the physician.
- If an HST is done through the dental office, remember, it should be used as a screening only -- not a diagnosis.
- Once the physician has diagnosed the OSA, ask his or her office for a copy of the PSG results and a prescription for an oral appliance therapy.
- Visit 2: Discuss the PSG results and the patient's expectations. Take impressions and a bite record for the appliance.
- Visit 3: Deliver appliance, verify fit and comfort. Have patient sign a consent to the possible occlusion changes.
- Visit 4: One to two weeks later, discuss signs and symptoms, check muscles and TMJ. Titrate appliance prn.
- Visit 5: Verify signs and symptoms. An HST can be done for titration purposes only.
- Refer back to their physician for follow-up PSGs with the appliance. The physician may want to perform a PSG or his or her own HST.
- Consider follow-up visits every six to 12 months. Report results to the patient's physician.
Guyton:: Finally, there are many appliance options to consider and they each have their own pros and cons -- it isn't a "one size fits all" approach. They must be appropriate for each patient and be FDA approved.
Poss:: Some common types of appliances are the SomnoMed Classic and their G-2. There is also the Herbst, the Suad for heavy bruxers, the TAP, Respire, The Moses and Myerson EMA Oral Appliances, and EMA. I suggest you personally make and wear every type of appliance that is made for your patients. This way you know how each appliance feels and how it works so that you can best understand your patients' needs -- because ultimately, that is what this is all about!
Conclusion:
We suggest the following three next steps:
- Attend some well-recognized courses and learn about sleep apnea treatment options. Consider learning more at sleepcomplete.com, sleepgs.com, lviglobal.com, and somnomedacademy.com. Some of our colleagues, Dr. Levy at lyonsgatepracticemanagement.com and Dr. Smith at sleepdallas.com, are also great resources for learning. Finally, look to join one or more of the following organizations: aadsm.org, acsdd.org, and aasmnet.org.
- Develop your internal office processes and build your referral network.
- Effectively market yourself to your community as an OSA solution.
Good luck in your OSA efforts!
Dr. Steve Poss maintains a private practice in Brentwood, Tenn., and lectures on cosmetic and sleep dentistry. Contact him at [email protected]. Brad Guyton, DDS, MBA, MPH, practices dentistry in Denver, Colo., and serves as COO of Jameson Management, alongside Misty Clark, VP of Creative Services. Jameson's team of 40 clinical, management, and marketing advisors improve the lives of dental professionals through niche in-office and virtual coaching, and marketing services. When you are ready to make your dream practice a reality, they can be reached at (877) 369.5558 or [email protected].
Past DE Issues