Q:
I thought I knew adequate information about prescribing pain medications for my patients, but I'm reading about many changes that appear to be completely different from what I've been prescribing. What's considered to be the "standard of care" for pain medications?
A:
Your question is certainly timely and important. Yes, the use of pain medications in all of the medical sciences is changing. You used the phrase "standard of care," which deserves a few words of definition. This phrase is often used in the legal sense, and there are somewhat confusing variations of the definition.
Standard of care (definition condensed from Wikipedia) is a treatment guideline that specifies appropriate treatment based on scientific evidence and collaboration between professionals involved in the treatment of a given condition. From the legal standpoint, standard of care is the level at which an ordinary, prudent professional with the same training and experience, in good standing, in a same or similar community would practice under the same or similar circumstances.
I've asked several large continuing education groups in different areas where I spoke what they're prescribing for the different levels of pain. The "standard of care" appeared to be similar in all areas. In summary, dentists have changed from the relatively routine use of opioid narcotic drugs to mainly over-the-counter drugs.
I will summarize the apparent standard of care for pain medications in dentistry later with a listing of medications for mild-to-moderate pain, moderate-to-severe pain, and severe pain.
Pain threshold
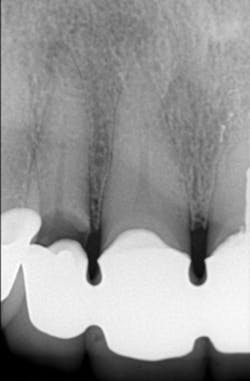
It is well known that all people perceive pain differently. Until you know the pain threshold of a specific patient, you cannot decide what level of analgesic to prescribe. The patient shown in Figures 1 and 2 had only an occasional awareness that there was movement in the grossly diseased mandibular molar tooth, while the patient with radiographically adequate endodontic treatment on a lower molar shown in Figure 3 was in constant pain, which interfered with his daily work. Pain threshold is obviously different from patient to patient. Dentists soon learn the pain thresholds of their patients.
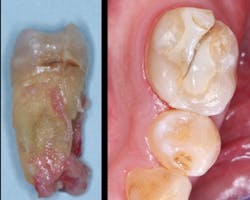
Figure 1: Mandibular molar of a patient who was aware of movement but who tolerated the mild discomfort for many months before seeking treatment
Figure 2: The molar shown in Figure 1 had obviously been in a state of degeneration for many months, but the patient did not have any significant disability related to the tooth. This patient had an extremely high pain threshold.
Pain threshold is defined as the least stimulus intensity at which a patient perceives pain. Every dentist knows that it varies hugely. What is mild pain to one patient can be severe pain to another.
Mild-to-moderate pain (Figure 3)
This relatively nondebilitating pain is the type that bothers someone, but it is usually tolerated at least for a short time. A good example of mild-to-moderate pain is seating a crown on a nonanesthetized patient. I have found that at least half of the patients having a full crown seated prefer to tolerate mild-to-moderate pain for a few seconds instead of enduring the pain of needle insertion and the lingering anesthetic result. This level of pain is not of major significance but is desirable to eliminate if the pain is expected to remain for days or longer.
Figure 3: Patient with apparently adequate endodontic treatment in mandibular molar who complained of moderate pain constantly.
Moderate-to-severe pain (figures 4-8)
You can easily determine when pain is moderate or severe. While you're operating, the patient indicates discomfort by grimacing, moving, or making a noise. When you suspect moderate-to-severe postoperative pain is likely, it is a good idea to prescribe an appropriate analgesic as related to that specific patient's pain threshold. When you do not know the pain threshold of a patient, I suggest prescribing an analgesic that you're confident will eliminate most of the pain in your patients who have the lowest pain threshold. Advise the patient that if the pain is tolerable or can be eliminated by low-level over-the-counter analgesics, they do not need to take the stronger analgesic. By so doing, you will not be bothered later with a call for a stronger analgesic.
Figure 4: Patient with splinted anterior crowns and large carious lesion on lateral incisor had moderate constant pain
Figure 5: Patient had moderate postoperative pain after tooth preparation appointment.
Figure 6: Patient had almost no postoperative pain after tooth preparation appointment. Both patients in Figures 5 and 6 had same apparent trauma during tooth preparation, but they reported very dissimilar postoperative pain.
Figure 7: This shows severe postoperative pain caused by removal of large lingual periapical infection on first molar.
Figure 8: Closed wound of patient in Figure 7 healed rapidly with diminishing pain after 24 hours.
Most commonly used analgesics for mild-to-mild-moderate pain
Note: See the February 2015 Clinicians Report Foundation publication for additional information. Available at www.cliniciansreport.org.
• Acetaminophen-500 mg every four hours or 650 mg every six hours, not to exceed 3,000 mg per day
• Ibuprofen-400 mg every four hours (over 400 mg is not better), not to exceed 2,400 mg per day
• Naproxen-500 mg or 550 mg two times per day
• Celebrex-400 mg, then 200 mg two times per day
Most commonly used analgesics for moderate-to-severe pain
• Ibuprofen 400 mg plus acetaminophen 500 mg, taken together every four to six hours with same limitations as above
• Celebrex 200 mg two times per day, taken with acetaminophen 300 mg to 500 mg every four or six hours, or 5 mg or 7.5 mg hydrocodone/acetaminophen, or 5 mg or 7.5 mg oxycodone/acetaminophen
• Hydrocodone 5 mg or 7.5 mg plus acetaminophen 300 mg to 325 mg
• Oxycodone 5 mg to 7.5 mg plus acetaminophen 300 mg to 325 mg
• Tylenol #3 or #4, which is 30 mg or 60 mg of codeine plus 300 mg acetaminophen
Most commonly used analgesics for severe pain
• Any NSAID (nonsteroidal, noninflammatory drugs) such as ibuprofen to hydrocodone, oxycodone, or Tylenol #3 or #4 as above. For example, use between doses of these medications.
• Hydrocodone or oxycodone 10 mg and 300 mg to 325 mg of acetaminophen
• Demerol 50 mg with maximum of 300 mg per day
Summary
Medications for dentistry have changed significantly in recent years. Some over-the-counter single drugs have been shown to be as effective or even more effective than narcotics, and they do not have the dangerous side effects or high cost of narcotics.
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics readers. If you would like to submit a question to Dr. Christensen, please send an email to [email protected].
Gordon J. Christensen, DDS, MSD, PhD, is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Dr. Rella Christensen) and CEO of Clinicians Report (formerly Clinical Research Associates).