Periodontal treatment or extraction and implant insertion?
by Carl E. Misch GS, DDS, MDS, PhD (h.c.)
and Jennifer T. Silc, DDS, MS
For more on this topic, go to www.dentaleconomics.com and search using the following key words: implants, ICOI, periodontal treatment, Dr. Carl Misch, Dr. Jennifer Silc.
Maintaining natural teeth in health, function, and esthetics is a primary goal of dentistry. In the past, the maintenance of a natural tooth was paramount, because tooth replacement techniques were costly and not as predictable as repairing the natural tooth. What is new in today's environment is that some dental procedures (as the treatment of severe periodontal disease, furcation treatment, or functional crown lengthening) may have a lower success rate or poorer cosmetic result compared to an implant to replace the tooth. Therefore, on occasion, the significantly compromised natural tooth may be extracted and replaced with an implant (right).
Implants should also be considered as an alternative when more expensive procedures are contemplated in an attempt to save or maintain a compromised tooth. Traditional methods to save a tooth have increased in cost over the years.
For example, multirooted endodontic therapy now approaches the cost of an implant surgery. When functional crown lengthening and endodontic post treatment is also required, the fees are usually greater than extraction and implant insertion. Treatment planning should take into consideration the natural tooth that requires periodontal therapy as well as multiple other aspects of treatment which compromise the long-term success and are cost prohibitive for the service provided.
A tooth may be considered for extraction because of prosthetic, endodontic, or periodontal considerations. On rare occasions, tooth extraction may even be considered rather than orthodontics to restore the teeth in a more esthetic or functional position. The primary discussions related to this article will be for periodontal considerations, which may warrant tooth extraction and implant restoration.
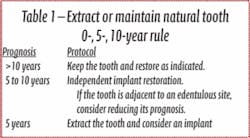
0-, 5-, 10-year rule
The dentist evaluates the natural teeth for their quality of health with widely used prosthetic, periodontal, and endodontic indexes. After this is accomplished, an estimate of longevity may be used to decide whether to extract or to treat and maintain the tooth, following a 0-, 5-, 10-year rule.
If the natural tooth has a favorable prognosis for more than 10 years (after it is returned to health), it is most often included in the treatment plan. The tooth under these conditions may even be considered to join an implant within the same prosthesis.
For example, the tooth may act as “a living pontic” in the final restoration, surrounded by sufficient implant support. The decision to use it or not as an abutment requires additional information, but few reasons support removal of the tooth to restore the partially edentulous patient.
A less than 5-year prognosis for a natural tooth despite restorative or periodontal therapy, warrants extraction of the tooth, with grafting and planning for implant abutment support as part of the initial treatment plan. This treatment scenario may often be faster, easier, less traumatic, and less expensive compared with maintaining a questionable tooth.
When probing depths are above 7 to 8 mm with bleeding upon probing, the teeth are usually placed in a 0- to 5-year prognosis. Maxillary molars with Grade II or III furca are at a higher risk of complications and are often lost within 5 years. If hygiene is poor with Grade II or III furca involvement in molars, the tooth most often is considered in the 0- to 5-year category. This is especially true when other teeth in the same quadrant are missing or hopeless.
A periodontal abscess results in rapid periodontal attachment loss and active bone destruction, and often reduces the longevity of a tooth. When a history of repeated abscess formation is observed from a tooth, a hopeless prognosis is usually assigned.
If the natural tooth prognosis (after periodontal, endodontic, or restorative therapy when necessary) is in the 5- to 10-year range, the treatment decisions are more nebulous.
In general, deep pocket depths of up to 7 to 8 mm with bleeding upon probing is an indicator of periodontal disease activity, and longitudinal studies suggest a poor prognosis. The teeth under these conditions may be placed in the 5- to 10-year category. Molars with Grade I furcation involvement often are also placed in the 5- to 10-year prognosis category.
Independent implant supported prostheses are indicated to replace any missing teeth in the 5- to 10-year category. The placement of as many implants as possible to support an independent prosthesis around the tooth, with treatment alternatives that will permit removal of the tooth without sacrificing the restoration, is indicated.
Of special note is teeth in the 5- to 10-year category next to a multiple edentulous site. A natural tooth distant from the future implant restoration is less likely to affect the implant reconstruction and alter the treatment sequences.
However, failure of a natural tooth adjacent to an implant site may cause failure of the adjacent implant and almost always (whether implant failure occurs or not) causes the restoration to be delayed and compromised. Therefore, if the practitioner is not sure whether the adjacent tooth to an edentulous site is in the 0- to 5-year or 5- to 10-year category, the tooth more often should be considered to have the poorer prognosis. Table 1 summarizes the decision making protocol involving a natural tooth abutment.
Discussion regarding periodontal disease
The severity of a periodontal problem may be such that extraction should be considered as the treatment choice to solve the disease. Severe periodontal disease may be addressed with extraction of questionable abutments more frequently than in the past, provided the resulting edentulous area offers sufficient bone for predictable endosteal implant placement and a predictable prognosis. Herodontics are discouraged when the prognosis is poor or failure of treatment may result in inadequate bone for implant placement.
Smoking is a major risk factor for periodontal disease progression, and smokers have an increased risk of developing periodontal disease compared to nonsmokers. Dental implants with a direct bone interface are less affected by smoking than the natural dentition. Therefore, extraction of the teeth in smokers with moderate to severe periodontal disease may be warranted followed by implant therapy.
Periodontal treatment may compromise implant therapy later. This is especially noted when the existing available bone around the tooth roots is compromised in height in the posterior mandible. An implant length of less than 9mm is less predictable than longer implants. It is more difficult to augment bone in height in the posterior mandible compared to other regions of the mouth.
Unsuccessful periodontal treatment and continued bone loss may render the remaining bone inadequate for placement of predictable implants. As a result, when 10 mm of bone height is all that remains from the mandibular canal to the remaining bone around the periodontally involved teeth, consideration is given to the predictable aspects of periodontal therapy.
Furcation involvement
The etiology of furcation involvements lead to a progressive and site-specific loss of attachment in most individuals. A Grade III furca indicates a through and through horizontal penetration of the probe. In general, Grade III furcation involved teeth present a poor prognosis, and regeneration of this type of defect is not predictable for most clinical situations. Therefore, teeth with Class III furcation have an unfavorable treatment outcome.
Furcation treatment of molars may include root amputation. The lowest success rate for root resection is found in mandibular distal root resections. Even when successful, to extract the distal root requires endodontics on the mesial root, core and crown of the mesial root, and the replacement of the distal root with an implant or fixed partial denture. An extraction of the entire molar and implant insertion has a higher success rate and often lower cost (see photos at right).
Mobility
While some authors have found that increased mobility is a factor that negatively influences the survival of a periodontally affected tooth, others describe no association between tooth mobility and treatment outcome. However, mobile teeth are poor prosthetic abutments to replace missing teeth.
When adjacent to a future implant site, the mobile tooth may cause the implant prosthesis to be overloaded. Therefore, the mobile tooth may be indicated for extraction, especially when in a molar situation and adjacent to an edentulous site.
Editor's Note: References available upon request.
Dr. Carl E. Misch is clinical professor and director of oral implantology at Temple Dental School in Philadelphia, Pa. He is also director of the Misch International Implant Institute. For more information, visit www.misch.com. Dr. Jennifer Silc is a diplomate of the American Board of Periodontology, and has a private practice limited to cosmetic periodontics and implant dentistry in Schaumburg, Ill. She is also an adjunct associate professor of Temple Dental School, and is a faculty member to the Misch International Implant Institute. For more information, visit www.woodfieldperiodontics.com.