by Karen Davis, RDH, BSDH
“Why should I learn the insurance codes? I just provide what the patient needs! The administrative team can worry about the codes.”
You don’t need to worry about the codes, but you do need to report them accurately. It’s critical. Let’s talk about why.
Understanding insurance codes - how they are defined and, more importantly, how the procedures should be used - is critical in order to accurately report nonsurgical treatment and assist the patient in obtaining maximum insurance reimbursement. This is true even for practices that do not accept assignment of insurance or file claims for the patient. Inaccurate reporting of procedures on an insurance claim can have legal ramifications if the insurance carrier questions the accuracy of those procedures. This can happen when a clinician provides “what the patient needs,” but leaves the administrative team with the task of selecting a code that may or may not reflect actual treatment (as in the case of prophylaxis vs. periodontal maintenance).
Due to so many variations of plans and the numerous restrictions written into insurance contracts, it is easy for confusion to set in or, worse, a tendency to let insurance companies dictate how we submit certain procedures when it comes to treating periodontal disease in many dental practices.
A good rule of thumb for insurance codes is to provide what the patient needs first, and then select the codes that most accurately describe your procedures. Establish clear referral guidelines between the general and periodontal practices prior to implementing nonsurgical protocols.
Let’s take a close look at how nonsurgical periodontal procedures should be implemented into patient care, but before we do, a word of caution for some of you. If you are a contractual provider for various insurance plans, application of this information may be different than for nonproviders.
Localized and generalized periodontal therapy
When it comes to selection of insurance code 4342, localized scaling and root planing per quadrant (periodontal therapy), or 4341, generalized scaling and root planing per quadrant, there is a lot of confusion both in treatment planning and reporting.
Too often, practices base fees and time allotted for periodontal therapy strictly on the numbers of teeth with pocketing and attachment loss in a given quadrant, which becomes a one-size-fits-all approach to treating disease.
For example, a patient who has only three teeth with minor attachment loss in a quadrant may also exhibit generalized hemorrhage on all other teeth within the same quadrant.
Therefore, rather than simply allotting time to treat three teeth - at perhaps half the time and half the fee of a full quadrant - treatment planning should be based upon how much time is required to treat all of the infection in any given quadrant, as well as provide adequate education and individualized oral hygiene instruction. Treatment planning would require further customization if the three teeth involved instead had moderate attachment loss, any furcation involvement, and/or if the patient had risk factors such as tobacco usage, diabetes, pregnancy, elevated stress levels, poor nutrition, genetic susceptibility, poor oral hygiene, occlusal disease, etc.
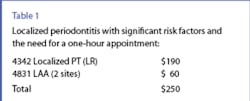
Note that while the actual scaling and root planing may take place only on the three teeth with attachment loss, all diseased sites should undergo definitive mechanical debridement to treat chronic periodontitis or gingivitis effectively. On occasion, procedure code 4342, for treating three teeth with attachment loss in one quadrant, actually requires the same amount of time and skill as procedure code 4341, for treating four or more teeth in a quadrant. If treatment requires a one-hour appointment due to the severity of the infection, depth and/or accessibility of the pockets, and overall risk factors, then the fee for 4342 should be equal to the same as a full quadrant of therapy (for example, $190, as shown in Table 1). Narratives can be included to insurance carriers noting extenuating circumstances for the time and fee.
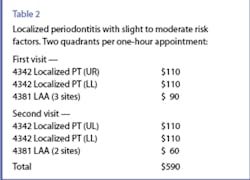
A more common protocol, however, is treatment of localized sites that occur in more than one quadrant. Often, two quadrants can be treated within a one-hour appointment when disease is detected early. If the fee for 4342, localized periodontal therapy, is $110 per quadrant, or approximately two-thirds the fee of $190 for a full quadrant of therapy, for example, two localized quadrants can be treated and billed within the same appointment (see Table 2).
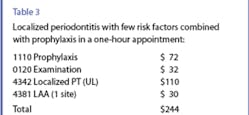
Some patients scheduled for a prophylaxis exhibit chronic periodontal infection on two or three teeth or sites only, so localized periodontal therapy could be provided in conjunction with a prophylaxis, preventing the need to return for a separate appointment since the rest of the mouth is healthy.
For example, a patient could be billed for 1110 Adult Prophylaxis, 4342 Localized Periodontal Therapy One to Three Teeth, and 0120 Periodic Examination all in the same appointment as seen in Table 3. If X-rays or locally applied antimicrobials are needed, those fees would be billed separately. Note: Prophylaxis and localized periodontal therapy can be provided on the same date, although when billed to insurance companies, many carriers only reimburse for one of the procedures. Consequently, patients should be informed about expected limitations for reimbursement.
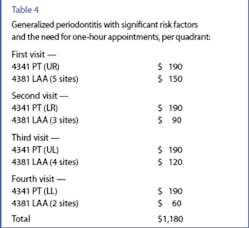
For patients with generalized periodontal disease with four or more teeth per quadrant, use procedure code 4341.
Table 4 shows a treatment plan for a patient who needs generalized periodontal therapy in all four quadrants and may or may not need a subsequent referral, depending on the tissue response to nonsurgical treatment.
Locally applied antimicrobials
Procedure code 4381 is used to report the use of locally applied antimicrobials, or LAAs, placed directly into diseased sites. LAAs should be placed at the time of therapy due to the fact that the pathogenic biofilm is at its lowest level, so healing takes place both from mechanical debridement and the addition of antimicrobials all at the same time. Studies revealing clinically significant benefits of LAAs were conducted with the agents placed at the time of scaling and root planing, rather than during reassessment or maintenance visits. Therefore, our clinical protocols should follow the same pattern, regardless of insurance reimbursement for these adjunctive agents.
Periodontal maintenance vs. prophylaxis
Once treated, patients with attachment loss and active disease should be maintained with procedure code 4910 (periodontal maintenance) for the lifetime of the dentition or implant replacements, according to the American Dental Association and the Academy of Periodontology. This includes patients with localized attachment loss. Prophylaxis is defined as a procedure intended to control local irritational factors. One could interpret that to mean plaque and calculus accumulations not associated with periodontal disease. Once periodontal infection is present as exhibited by bleeding tissue, permanent bone loss, possible furcation, and/or tooth mobility, periodontal maintenance following treatment is intended to assist patients in controlling this disease which can be episodic and site-specific throughout their lifetime.
What about patients who have only two teeth with attachment loss, and once treated remain periodontally stable? Are there ever any “exceptions to the rule” of 4910 periodontal maintenance following periodontal therapy for the lifetime of the dentition? While both the ADA and the AAP use very clear language to describe periodontal maintenance - “for the lifetime of the dentition” - which would apply to the vast majority of cases, clinical judgment of the dentist may determine an exception to the rule, so to speak, in very individualized cases.
For example, for a patient diagnosed and treated for localized periodontal infection with localized minimal attachment loss around two teeth only who responded with excellent clinical results, maintained those results without relapse of the disease for 24 months following therapy, and had no additional risk factors increasing his or her susceptibility to disease, a new diagnosis could be made by the dentist to maintain the patient’s status through customized intervals of prophylaxis instead of periodontal maintenance. That being said, caution should be taken never to give in to the temptation to “switch” a patient back to prophylaxis simply because it improves insurance reimbursement! Studies repeatedly confirm that periodontal patients benefit from definitive periodontal maintenance procedures following active therapy, which, when performed at close intervals, help to control the disease, thereby saving the patient dollars in the long run. Clinically, our goal should be to educate patients about the distinctive differences between periodontal maintenance and prophylaxis, thus increasing the value of the procedures, which we know are often not reimbursed at the frequency or the amount the patient desires or needs.
Establish a healthy team to dispel the confusion
Patients will ask any team member questions about various procedures. Therefore, it is critical that everyone on the team has a clear understanding of the services provided in the hygiene department and why. A great place to start is to have a team meeting with the 2007-2008 ADA Current Dental Terminology and explore the definitions of these procedures together. Next, make it a priority to carefully screen all team members for signs of periodontal disease and provide therapeutic treatment as indicated! Truly valuing our patients’ health begins with valuing our own.
Dispelling confusion about insurance codes, benefits, and procedures enables the team to focus on patients’ needs, treat the disease appropriately, and build value for a lifetime of dental hygiene services regardless of insurance benefits.Karen Davis is founder of Cutting Edge Concepts®, is a consultant with The JP Institute of San Diego, Calif., and is still practicing hygiene after 28 years. An international speaker, she challenges audiences to “think outside their boxes,” and has authored numerous articles related to practicing comprehensively. Contact her at [email protected] or (972) 669-1555.