Pat Carter and Jeff Carter, DDS
Most people would agree that designing an effective dental facility requires an intimate understanding of dentistry and a thoughtful identification of the design objectives for a specific practice. That statement alone involves a multitude of details and design decisions that can be quite overwhelming (assuming you want to attend to all the details and get it "right"). And while that is the primary part of the designing process, evolving factors outside of the control of practitioners will greatly impact the design and economics of current and future facilities.
What are some of those factors?
• Regulatory factors
In the early 1990s, the Occupational Safety and Health Administration (OSHA) regulations required appropriate labeling, storage, and inventory access to certain regulated dental materials and drugs. It also mandated protective eyewear, gloves, and gowns for the dental staff; appropriate disposal of biohazardous materials; and compliance with sterilization processes to protect the general public (your patients). In response, dental office design began to include appropriately sized and accessible storage and inventory areas, staff areas with changing rooms and storage for gowns, appropriately labeled and located disposal drops, and thoughtfully conceived central sterilization areas.
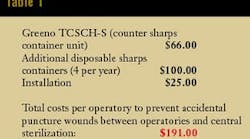
A specific example of a design response to OSHA regulation is the placement of a "sharps" receptacle in each operatory and the sterilization area. Rather than transporting contaminated needles or scalpel blades to a centralized sterilization area, disposal now occurs in the room where the sharp was used. The rationale is to prevent contaminated "sharps" from being dropped or misplaced en route to sterilization. A needle on an operatory floor can conceivably puncture an exposed foot or puncture a retrieving hand (gloved or ungloved). A recessed sharps disposal on a countertop with a minimally visible grommet ring is an excellent solution to this requirement. Companies such as Greeno provide these solutions. Table 1 shows an example of the cost implications of this requirement.
Dental industry veterans understand that the evolution of these OSHA safeguards decreases the likelihood of disease transmission in dental facilities and the diseases associated with those promulgated regulations. Receiving periodical empirical evidence of the success of these regulations would also be meaningful to the dental community as a counterpoint to the increased costs absorbed by all participants in the delivery of dental treatment.
By the end of the 1990s, the ADA (the American with Disabilities Act) inserted regulations that addressed disabled patients and disabled staff members in the dental office. The generally understood handicap code plan configurations no longer met the expanded patient and staff accessibility requirements imposed by the ADA. This law has profoundly impacted the arrangement of space and the amount of square footage required to effectively design an ADA-compliant dental office. A four-operatory office that seemed spacious at 1,500 square feet now may require 1,800 to 2,000 square feet to comply with ADA accessibility regulations.
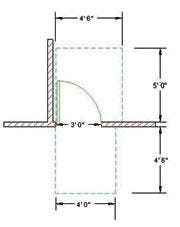
Dental office floor plans that are ADA-compliant are confusing because they seem to waste precious and costly space in unusual locations. ADA compliance requires any door within your facility to have an 18-inch clearance between the door opening side (not hinge side) and a wall if the door swings inward. This is considered the "pull" side of the door. On the other side of the door — the "push" side — ADA regulations require a 12-inch clearance. These clearances allow wheelchair-bound patients to position themselves to one side of the door and swing the door past without colliding with the wheelchair. This requirement is what drives the minimum size of compliant rooms; however, it can create the undesirable effect of doors swinging out into corridors because sizing does not allow an 18-inch door clearance inside a space. For example, the smallest room you can have in a dental facility and still swing the door into the room is 5 feet by 5 feet. This assumes there are no fixed objects in the room. As soon as you introduce a standard, 24-inch deep, fixed countertop to one end of this 5 feet by 5 feet space, ADA-compliance would dictate its size to increase to 5 feet by 7 feet or even larger, depending on spatial use and local ADA interpretation.
You can reasonably calculate the increased square footage assumptions of ADA-compliant dental facilities based on the number of doors within the facility. An ADA-compliant dental office door swing consumes approximately 45 sf compared with a non-ADA compliant door swing of approximately 25 sf. If a five-operatory facility has 15 doors, the square footage increase due to ADA compliant door swings is (15 sf x (45 sf - 25 sf) = 300 sf), an additional 300 square feet. If your existing five-operatory facility has 2,400 sf and was constructed pre-ADA, an exact duplication of your existing plan conceivably would require 2,700 sf to comply with today's standards. If interior finish-out construction costs for well-designed dental facilities range from $80 to $140 per square foot, you can better appreciate the cost implications of your project from an ADA-compliance standpoint.
ADA compliance also mandates wheelchair ramps for elevation changes and elevator access to dental facilities located on multiple levels. A hydraulic elevator for most two- or three-story dental facilities typically costs around $50,000. Wheelchair ramps require 10 to 12 feet of ramp for every 12 inches of rise. A four-foot rise from your parking area to your patient entry door typically would require a 40-foot ramp with appropriate railing. This same ramp costs approximately $20,000 to $30,000.
Do people in wheelchairs deserve equal access to dental facilities? Absolutely. Do participants in the delivery of dental care that share the increased costs associated with ADA compliance deserve to be thanked ... yes!
Compliance with these regulations applies to all dental offices designed today. It is wise to engage design and construction professionals who understand these regulations. Otherwise, rejection, revision requirements for drawings, or worse, tagging (stopping construction) on a job site by an inspector for noncompliance is an unfortunate and costly possibility.
After you address these OSHA and ADA requirements in your dental office design, what other noteworthy changes in dental office design today should you address?
• HIPAA compliance
Understanding the compliance implications of this privacy act has fostered forums, articles, and fervent discussions within the dental community. The intent of this law and the subsequent compliance steps that dentists should take are still under development by the agencies assigned to regulate this act. The American Dental Association is pressing for these compliance determinations so that it can appropriately inform its membership. And, even now, consensus is developing on the specifics of patient file information compliances. However, compliance is not limited to the administration and exchange of patient file information. The visibility and auditory patient privacy directives of the HIPAA are affecting the dental office design criteria in a number of areas.
Sound and noise concerns that have plagued staff in front-desk areas will now become HIPAA noncompliance issues. The ability for patients to interact with front-desk personnel in greater privacy is now a HIPAA design consideration. Separation of the appointing activity from the waiting area and easy access to a private consultation room will effectively address this issue. Introducing a consultation room into the dental office has become a design compliance response that protects the dialogue between the dentist and the patient about procedural, medical, and financial issues. Computer monitors also must be positioned out-of-view (across a desk or across a room) in a such a way that personal information about one patient is not visible to another patient nearby.
Surprisingly, the cost implications of HIPAA on well-designed dental facilities are minimal. For years, we have advocated consultation rooms and semi-private areas to facilitate private conversations; architecture and finish materials to minimize sound transmission; and protecting the confidential patient information that is displayed on monitors. Not surprisingly, less well-conceived facilities are suffering the greatest increased costs to achieve HIPAA compliance.
• Amalgam separators
The most recent regulatory issue to influence design is the use of amalgam separators. As with any new issue, confusion abounds. The short explanation would recommend amalgam separators be plumbed at the confluence of all vacuum lines and before the holding tank (semi-dry units) or vacuum pump (water-driven impellers). This allows heavy metal separation based on weight and filters out any amalgam particles before they can enter the municipal sewer system. RamVac, the dental industry leader in vacuum pumps, provides an amalgam separator unit for approximately $700. Removable filters ($100) are changed two or three times a year and disposed through biohazardous protocols. Amalgam separators are not large and would consume approximately two cubic feet of space.
What nonregulatory factors are currently influencing design?
• Technology
Technology in the dental office is no longer an afterthought. Dealing with dental technology after the office is designed, or worse, after construction is completed, translates to offices with exposed cable runs, compromised operator access to technology, and / or technology purchases that either fall short or far exceed the needs of the practice.
For these reasons, planning for and installing the cabling "system" to support current or future technology should be a part of the facility design process. That said, a word of caution is warranted about which company you choose for your technology design and development. This design arena is still rife with technology companies that know a lot about "high tech" but little about its specific application to dentistry. In our observation, the result is system installations that far surpass dental application requirements and the abilities or objectives of the dental staff end users. Our recent review of submitted specifications and pricing to clients confirm that these circumstances still exist. Therefore, be sure to retain the services of a reputable firm that specializes in dental technology applications. By doing this, you are more assured of appropriate equipment specification and installations that support your dental objectives rather than straining the dental practice financially for the sake of "technology."
An industry rule of thumb for cost approximations of networked computers within a dental office is to assume $5000 for each networked computer in your facility, which includes all costs for computer hardware, software, networking, cabling, mounting solutions, and installation. However, this $5,000 assumption does not include dental specific technologies layered over the more generic computer infrastructure. If your new, five-operatory facility needs 12 computers, you can expect to invest approximately $60,000 for just the computer network infrastructure.
• Operatories — size and access
Considering our background, it is interesting to examine the changes occurring in the dental operatory, primarily because the 9'6" x 10' operatory has been a "mainstay" in dental design for a long time. We, too, have promoted this size as optimum for the general practitioner for many years and for valid reasons. However, the expansion into more complex dental procedures, the material requirements involved in these procedures, the increased size in dental chairs, the heightened demand by operators for mobility at the chair, and the need for access to technology that supports this treatment command a different design response.
Therefore, another change we promote in dental design is the development of an optimally sized operatory to meet the specific type of practice rather than assuming the "standard" operatory design solution. For example, in a high-volume general practice that emphasizes family dentistry or smaller cosmetic and restorative procedures, the demand for a larger operatory or additional storage cabinetry may not apply. However, for the practice focused on large-case, advanced restorative procedures, the operatory size, cabinetry storage, and access will be different. The addition of overhead side cabinets to accommodate infection control and restorative materials may generate additional costs of $1,500 to $2,000 per operatory.
• Central sterilization
Central sterilization still is an effective design solution for instrumentation delivery to the operatory. OSHA reinforced these concepts by mandating appropriate sterilization processes as a compliance requirement. Even so, the expansion of material requirements necessary to effectively complete advanced dental procedures have challenged the notion that everything procedural must be delivered via a tray from a central location.
We still maintain that all instruments and handpieces that require sterilization are stored, organized, and delivered most effectively via tray set up to the operatory. Basic consumables also can be stored and delivered effectively in tray set-ups as well. We also agree that to be effective, central sterilization areas still require an appropriate amount of linear feet of counter or cabinet space to support proper sterilization procedures.
The exception will be with the persistent premise that all materials utilized in dental procedures must be stored in the central sterilization area and delivered to the operatory in tubs or trays. A multitude of adhesive, restorative and impression materials, and "guns" are accessed in many practices regularly. But retrieving materials of considerable mass and/or number through central tubs can be inefficient and outdated. For example, you wouldn't want to retrieve three tubs for every crown preparation. Design must respond with appropriate solutions to support the efficient access and utilization of these materials within the operatory.
Cabinetry in the sterilization area may actually decrease as we shift materials storage back to the operatory. Removing 10 linear feet of glass-front overhead cabinets can save approximately $3,500. This cost savings can help offset the increased costs of operatory expansion.
• Dental staffing
Management consultants predict significant changes in administrative staffing with the onset of computer scheduling and business systems. The type of dentistry produced affects the type and number of personnel required to execute it. In addition, the onset of computerization has also increased staff productivity, reducing the number of personnel needed to run a dental practice.
We find that working closely with management consultants and their clients is a great way to identify the spatial needs for the front desk and business areas. Anticipating current and future staff needs is an important design decision that must be made for practices to develop effective, efficient administrative space.
• Digital dentistry: Is the darkroom gone?
Our clients regularly pose the question of whether to incorporate a darkroom. The impulse is to respond in the affirmative and assume a darkroom will be used for something else when the office "goes digital," or, conversely, to assume the office will be completely "digital" from the beginning, rendering a darkroom unnecessary. The better response might be "How committed are you to going digital and how soon?"
Creating a darkroom within your office means creating another ADA-compliant space where square footage is considered. And if this space is an anticipated dinosaur, then the more appropriate design response may be to locate an auto-processor with a daylight loader in an alcove (without a door and without an ADA- access issue) that also has been designed as a future digital scanning/workstation (CPU/keyboard) area.
Scanning technologies (DenOptix, Scan-X, and others) are emerging as a more affordable and reliable technology than the hard-wired sensors options originally introduced into the dental market place. This makes the above design solution the one of choice for those dentists who are still using film, but seriously contemplating the leap into digital radiography in their future.
• Consultation rooms
The consultation room has become an accepted design "concept" for the practitioner who understands the benefit of a space devoted to treatment presentation and consultation. Management consultants helped us understand this concept many years ago, and HIPAA's privacy compliance edicts have reinforced it further. Space permitting, most dentists prefer this design solution.
Easy access to case presentation technology (a computer workstation) and a comfortable presentation environment are primary design criteria. Unfortunately, design solutions for the consultation room often fail to incorporate both considerations. The table-and-chairs-arrangement in the middle of the room reduces access to technology on the side counter, making it a less effective solution. Alternatively, built-in cabinetry with a table peninsula that gives both dentists and patient visual access to a computer workstation during treatment presentations addresses both issues optimally.
• The staff room
"Why in the world do we need a staff room?" has been a typical response to the idea of incorporating a separate area for staff use. Management consultants again deserve credit for convincing dentists that staff rooms are more than just a frivolous expense. This paradigm shift has been realized in many successful practices that understand that a supported staff is a supported practice.
When updating your staff room criteria, consider the technology available. Beyond lunch room and morning huddles, the practice can benefit from flexible furnishings that allow tables to be folded and removed, stacking chairs that can be arranged for workshops and then put away, and LCD projectors and pull down screens installed in cabinetry for presentations.
Whether looking within the practice, complying with outside regulatory factors, or integrating the latest in equipment and technology, the design of an effective dental facility responds to the criteria that is detailed and understood. For your part, be thoughtful about your practice objectives and expectations. Ultimately, the ideal office for you should be a direct response to you as a practitioner, to the type of practice you have now and want in the future, and to the community that it will serve. In this way, design helps to make your ideal office a reality.