Navigating Medical Billing for Dental Sleep Medicine: It's the wildest ride in the wilderness
In this first articleof a quarterly series, Erin Elliott, DDS, explains the paperwork needed for medical billing prior to a consultation for dental sleep medicine. Part 2 of this series will appear in our September issue.
When I began my journey in dental sleep medicine six years ago, I couldn't wait to implement this new, life-changing service in my office. There was only one problem: I had no idea how to navigate the hurdle of billing medical insurance.
So I decided not to bill patients' insurance. I didn't want to deal with the learning curve. Instead, I charged sleep patients up front so they could handle the billing. Do you know how many sleep appliances I did? One per month-if that. I knew dental sleep medicine was a needed service for many, and I was one of the first dentists in the area to offer it. I wanted to do more and help more. Once I became one of the first Medicare providers in early 2011, I realized I couldn't avoid medical billing anymore. My staff and I had to learn it.
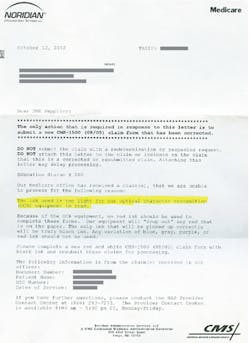
I decided we could teach ourselves. How hard could it be? I was billing only one diagnosis code and one treatment code, right? We thought we were ready to roll when we bought a dental sleep medicine software program and the correct paper from the proper government entity. Off to the presses we went!
. . . Until we got denials because the ink was too light or because the X was one millimeter off. Egad! It was so frustrating, and it illustrates the exact reason why patients are not getting more of the help they need. Dentists across the United States have told me they are not even considering dental sleep medicine training because they don't want to bill medical insurance.
Join me now and in upcoming issues of Dental Economics as I walk you through tales from my journey to help you avoid some of the mistakes I've made and navigate the pitfalls of billing medical insurance.
In-network, out-of-network, GAP exceptions, durable medical equipment (DME), Medicare-participating versus -nonparticipating, accepting assignment, Part B, ICD-9 versus ICD-10, peer-to-peers, appeals, denials . . . Hold on to your hats and glasses 'cause this here's the wildest ride in the wilderness! Oh wait—that's Big Thunder Mountain Railroad at Disneyland. Just as I survived that ride growing up, I think you will be able to handle this next part.
In this first article, let's discuss all of the paperwork you will need before a patient even walks in the door for a consultation. We have a special intake form that asks what the patient's demographics are, who the primary care doctor is, where the sleep study was done, and most importantly, what type of medical insurance is to be used. The staff member who took the phone call and scheduled the patient is in charge of "closing the loop," as we say at my office, by tracking down the sleep study, sending the patient the paperwork or the link to complete it online, and sending a request to the third-party biller for the verification of benefits (VOB) or insurance verification (IV). Basically, the verification tells us if the codes are covered, what the in-network or out-of-network benefits are, if a preauthorization is required, and how much of the patient's deductible has been met.
My goodness, I love November and December when most patients are eager to move forward with treatment because their out-of-pocket responsibilities are minimal. As you may know, the deductibles are different in the medical insurance world. In dental, we have a maximum benefit, so patients hold off on treatment until January if they have met the benefit maximum. But in the medical realm, patients must meet a minimum requirement for the out-of-pocket costs to be reduced. Add in health savings accounts (HSAs), and patients really want to proceed with treatment.
Whether it is a patient of record or a patient from an external referral or external marketing, we always schedule a separate consultation appointment. First of all, the hygienists don't want me to get into a 10-minute conversation with a patient in one of their operatories if another patient is scheduled to come in. It also helps us to be prepared for the patient, and the patient is better prepared to receive the information. I detailed our consultation process in the Dental Economics sleep apnea issue, but essentially, this is how it works: My assistant reviews the patient's chief complaint and uses an iPad presentation I've created to give the patient an overview of obstructive sleep apnea, the health consequences, the treatment options, and how oral appliances work. Then I review the patient's sleep study and do an exam. Prior to proceeding with impressions (we try to take impressions the same day), my financial arrangement team member enters to review the patient's medical insurance. It is our goal to minimize patient out-of-pocket responsibilities, but it is important that we know the deductible, how much of it has been met, and what the co-pay will be. We can find that information by using a third-party biller or the online portal that most insurance companies provide. You can start by asking your local rep.
The goal of this first article was to give you an overview of how complicated implementing dental sleep medicine can be. But I also wanted to show you that if you learn the medical billing "language" and use a tour guide, you can navigate this ride to provide a valuable service to your practice and your community. So hang on tight and join me in the coming months to explore some of the crossroads, hills, curves, and valleys that I have encountered and survived!
Erin Elliott, DDS, is a practicing general dentist in Post Falls, Idaho, where she has successfully integrated dental sleep medicine into her busy general practice. She lectures extensively and leads a hands-on workshop focusing on practical strategies for successful implementation into the busy general practice. She is an active member of the American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine. She is the president and a diplomate of the American Sleep and Breathing Academy. She can be contacted directly at [email protected].