Why do I need cone beam?
Q:
For the last several years, I have seen articles about cone beam computed tomography (CBCT) routinely. I also see ads in almost every journal for these $100,000+ devices. I am still hesitant to purchase one, since I have been getting along very well without using cone beam for nearly 20 years. I know that Clinicians Report Foundation, with which you work, stresses practical concepts and devices. Should I get a cone beam device, or is it just another expensive and elective technology?
A:
I had many years of practicing prosthodontics without the use of cone beam, and I did not know what I was missing. However, I agree with you that many of the highly promoted technologies are quite elective and the procedures for which they are promoted can be accomplished well using conventional concepts. That is not the case with cone beam.
We have now had cone beam in our clinic for more than 13 years. My candid statement about its value can be summed up easily by the following sentence. I don't know how we survived clinically before we started using this highly useful technology.
ALSO BY DR. GORDON CHRISTENSEN |The best way to connect a crown to an implant
I assume you are a general dentist. If that is the case, we know the techniques that general dentists accomplish. Let's review concepts commonly accomplished by general dentists and how they relate to cone beam use. I hope that my comments will demonstrate the value of this technology for typical general dentists.
Implants
It is well known that only a small percentage of GPs place implants in the United States. I have tried for 20 years to remedy that challenge, which is not present in many other developed counties. I am pleased to see that, currently, many implant companies are present in the United States, and GP placement of implants is on a steep rise. In spite of the fact that many GPs do not place implants, almost all GPs diagnose and treatment plan for implant placement and subsequently restore them.
The most common use of cone beam is to diagnose, treatment plan, and place implants. I have personally placed and restored implants for about 30 years. For most of those years, I did not have cone beam. Did I know exactly where the implants should be placed? Could I be assured that I had placed the implants without infringing on the known vital structures or perforated the bone? The answer is no.
You may or may not be placing implants, but you most assuredly are diagnosing whether implant placement is possible for specific patients. Does cone beam help?
In my practice, when treatment planning for implants, I observe the cone beam images together with a dental assistant and the patient. The patient receives from us an introductory education about the related oral anatomy, and it is gratifying to see him or her understand the potential plan by observing the 3-D images. The patient actually helps with the treatment plan. I feel strongly that an educated patient is much more accepting and calm during treatment than one who knows nothing about what you are planning to accomplish or about the treatment you are going to refer to another practitioner.
ALSO BY DR. GORDON CHRISTENSEN | Ask Dr. Christensen: Gray- and black-market products are increasing
If you are placing implants, using a surgical guide to assist in placing some of the implants is relatively easy, not very expensive, and certainly helpful for a practitioner who is just learning to place implants (figures 1 and 2).
Figures 1 and 2: This cast represents a patient who has two missing maxillary lateral incisors. The surgical guide was made as an educational model showing use or nonuse of a guide. One of the implants was placed using a guide and the other missing tooth was replaced using freehand implant placement. Surgical guides are very valuable for practitioners just beginning implant placement and for complicated clinical situations, but most implants are placed freehand using radiographs as a visual guide.
Impacted tooth removal
Diagnosis and treatment for third-molar impactions is reported to be the second most frequent use of cone beam. CR Foundation surveys show that more than 50% of GPs remove impacted third molars. It is well known that third-molar removal is one of the most frequent techniques that is challenged legally. Can you tell where the roots of a third molar are located? Are the roots facial or lingual to the inferior alveolar canal? If you break off a root tip, where is it located in a 3-D orientation? Two-dimensional radiographs are extremely helpful in many situations, but 3-D views as shown in Figure 3 add highly useful views in many dimensions, including facial-lingual, more predictability, and a better clinical result.
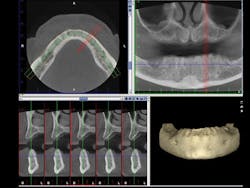
Figure 3: An example cone beam image shows in the upper right image the typical 2-D view of the maxilla and mandible. The lower left image shows the maxilla and mandible view 90 degrees from the upper right image. Planning for implant placement is greatly improved by cone beam images.
Endodontic treatment
General dentists accomplish the vast majority of endodontic treatment in the United States. This treatment is reported to be the third most frequent use of cone beam. Endodontists, who are the leaders and teachers for endodontic treatment, are now using cone beam routinely. What are some of the reasons for this use? All of us occasionally have a patient with an endodontically treated tooth that appears on a 2-D radiograph to have received excellent endodontic treatment, but the patient still has discomfort. You know the various potential reasons for this treatment failure, but can you visually determine them? Is the tooth cracked? Is there another root or another canal that you cannot see on a 2-D image? Do overlapping roots disguise a problem or condition that could easily be seen on a 3-D image (figures 4-6)? It is easy to predict that cone beam will soon become recognized as being necessary for predictable endodontic diagnosis and treatment.
Figures 4-6: These images provided by Dale Miles, DDS, MS, show a lower right second molar with multiple roots. It is apparent that a 2-D view would be inadequate to provide enough information for appropriate endodontic treatment.
Miscellaneous uses
The three apparent major current uses for cone beam have been described above. As this technology becomes more widely available, other uses will be developed. It has become a standard procedure for our practice to use cone beam images for many other tasks such as:
• CAD/CAM devices such as 3-D orthodontic models
• Inferior alveolar nerve location
• Sinus location
• Odontogenic lesion location
• Surgical guide construction
• Trauma evaluation
• TMJ visualization
• Numerous others
Access to cone beam images
The current cost of cone beam is a challenge for dentists who recognize the value of this technology but cannot afford to buy a machine. There are a few ways to have access to cone beam images:
• Buy a device. This is beyond the financial ability of many dentists who are still recovering from the lingering recession.
• You and another dentist or dentists buy a device and share its use. This is a very viable alternative, although the American Dental Association estimates that approximately 60% of dentists are in solo practice and do not practice with another dentist.
• Use a mobile radiographic clinic in your area. Some geographic locations have mobile imaging facilities and staff who will be pleased to come to your area and provide images and their interpretation for you.
• Use a radiographic imaging clinic in your area. These clinics function in at least two ways. You may have your patients go to the clinic, have an image made, and you interpret it . . . or you may have the image made and interpreted by someone in the clinic or elsewhere. Please remember that you are legally liable for interpretation of the structures and the pathology present on the images. Taking a course on cone beam interpretation is highly important as practitioners incorporate cone beam into their practices. Using the services of an oral and maxillofacial radiologist for reading the images is also a very good alternative.
Summary
Cone beam imaging is no longer just coming; it is here now! Those practitioners who have implemented this technology find that it is indispensable. The positive characteristics of cone beam are well known, but the expense, learning curve to use it, and denial of the need for it have slowed cone beam acceptance. I strongly suggest that dentists at least find access to cone beam, and that it will not be long until they recognize its value and purchase a cone beam device.
Gordon J. Christensen, DDS, MSD, PhD, is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Dr. Rella Christensen) and CEO of Clinicians Report (formerly Clinical Research Associates).