The Bulk of the Matter in Composite Restorations
By John C. Comisi, DDS, MAGD
The restoration of dentition with resin-based composite (RBC) has been a staple of the dental professional for many years. The wonderful esthetics and ability to create lifelike restorations has made a major difference in the creative and healing process we carry out each day in our offices. But these very same materials have also created some dilemmas in the final results we are able to achieve.
The reality is, all composites shrink. This is, of course, caused by the polymerization of the resin material. But in an effort to reduce the amount of time per procedure, many dentists would work with these original materials in "creative" ways that were contrary to how these materials were designed or indicated for use.
Placement of material in increments greater than the recommended 2-mm layers became a relatively commonplace practice, and with that, challenges to the overall well-being and integrity of the dental restorations began to be reported.
Sensitivity, marginal gaps, and restorative failures became commonplace due to internal stresses that developed. This was caused by the polymerization of the material. These original resin-based composites' physical properties and composition (the resins and fillers used) were not designed to be cured in large, "bulk" increments.
Additionally, the coefficients of thermal expansion, modulus of elasticity, water absorption, and solubility of these original materials created problems.
Recognizing this problem, researchers explored ways to make these materials better. It was found that the fillers in our resin-based composites helped to improve the physical properties of these materials. The characteristics of each RBC material, it was found, are a result of the filler material. The surface of the material, the size, shape, filler load, modifiers, size, and distribution of the fillers added to the resin create unique qualities that shape what an RBC can and cannot do. In fact, the fillers are an important factor in helping to reduce the shrinkage in our RBCs.
Concurrently, development of newer resins with unique mixtures of monomers were being developed that can help to improve biocompatibility and further enhance the physical properties of the material.
As these advances were made in the science of resin-based composites, multifunctional composites with novel microstructures were developed. The importance of nanotechnology in this advancement cannot be overemphasized. Nanotechnology involves the production of functional materials and structures in the range of 0.1 to 100 nanometers via various physical or chemical methods.
These nanomaterials can be tailored to create new classes of composite materials with improved properties. The inclusion of various types of nanofillers and nanofibers into dental composites and bonding agents has improved the physical properties: strength, polishability, wear resistance, esthetics (by improving the light scattering), and bond strengths in many dental applications.
The incorporation and use of these nanoparticles in the form of nanorods, nanofibers, nanospheres, nanotubes, and ormocers (organically modified ceramics) into dental restorative and bonding agents can create more biomimetic (lifelike) restorations.
This will not only enable these materials to mimic the physical characteristics of the tooth structure, but will also be able to facilitate the remineralization of that structure and can help to reduce the biofilm buildup.
Bulk-fill materials made their first appearance in the dental world in 2009, much to the delight of the dental clinician. This would help them do direct restorations quicker and easier. These original systems were designed to use these new filler types and resins and to be highly translucent to enable greater depth of cure; however, the translucency that enabled greater depth of cure was not very esthetic and could not match surrounding tooth structure.
Several other products were introduced with lower filler content to overcome this translucency issue and allow for more light penetration and curing depth. This, by the very nature of lower filler content, can be problematic in the final restoration.
Yet, other products were developed that found ways to alter the chemistry of the RBC to create an environment that helps to enhance the ability of the polymerization by acting as a catalyst. Thereby, this increases the cure of the material once it starts.
Many of these materials created great polymerization and shrinkage stress, and often had a high occurrence of voids due to their inability to flow well. As always, further research and efforts were made by the dental industry to help overcome these shortfalls in these materials.
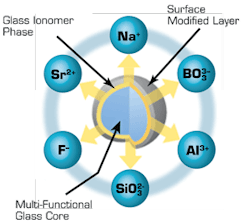
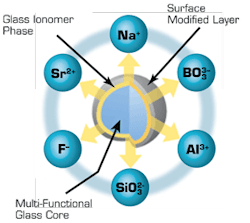
One of the solutions proposed is the use of Giomer Technology, introduced by Shofu Dental, which incorporates a Surface-Partially Reacted Glass (S-PRG) Filler Particle. This is a bioactive, tri-laminar structure with a multifunctional glass core embedded in a resin matrix (Fig. 1) that is available in various Shofu products. These products include the Beautifil® line of products.
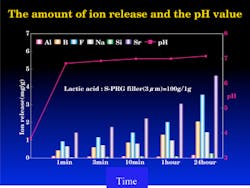
The S-PRG fillers have been shown to release six different ions, including fluoride, from the glass core. Additionally, the material can be recharged with fluoride to help with remineralization and protection of the dentition in a manner similar to glass ionomer materials.
This release of ions from the giomer has also been shown to neutralize the acidity of the oral cavity and contributes to the creation of an anti-plaque effect in areas adjacent to giomer restorations.
Long-term in vitro studies at the University of Florida have been published regarding these unique properties. The first paper published on this in JADA 2007 followed individuals who had Class I and Class II restorations placed using these giomer materials.
At the end of eight years, there were no failures, no secondary caries, no postop sensitivity noted, and a high level of esthetics maintained. The 13-year follow-up to these same people and restorations found a 66% retention rate and a secondary caries rate of 3.27%.
With this knowledge of long-term effectiveness, Shofu has introduced Beautifil®-Bulk Flowable material, which can add a new dimension to the direct bulk fill restorative landscape. The company reports that the S-PRG filler in this product allows for an ideal balance of light-diffusion and transmission.
This enables a 4-mm depth of cure of the material, and at the same time, creates optimal opacity to help match and mimic the surrounding tooth structure to enable a chameleon effect in the final restoration.
The dense distribution of filler in the resin matrix (72.5 wt%) is reported to successfully reduce polymerization shrinkage and shrinkage stress, and as such, can help to greatly improve marginal integrity and reduce postoperative sensitivity when placing a direct bulk material. The flow of the material is reported to be dense, yet easy to place.
Additionally, the material has nice handling properties that allow easy placement in the cavity preparation. This reduces the risk of voids, and the material stays where you place it without any slumping. This is a feature the clinician will find attractive in clinical use.
Beautifil®-Bulk Flowable material is indicated for use as a base/liner in Class I and Class II direct restorations in 4-mm increments, and then covered with a final restorative material. It can also be used as a final restorative material in small, posterior, minimally invasive occlusal defects.
What has made all the Beautifil® line of materials interesting in the past is the easy-to-use, bioactive, acid neutralization, protective abilities of these restorative materials.
The introduction of Beautifil®-Bulk Flowable material offers the clinician a potential advantage of creating quick, direct, bulk-fill, bioactive restorations incorporating protective properties that many will find beneficial in direct restoration procedures.
Please search for "John Comisi" on www.dentistryiq.com. for more information.
References
1. Sumita B. Mitra, Ph.D., M.Sc., Dong Wu, Ph.D. and Brian N. Holmes, Ph.D. An application of nanotechnology in advanced dental materials. The Journal of the American Dental Association October 1, 2003 vol. 134 no. 10 1382-1390.
2. Saunders Scott A. Current practicality of nanotechnology in dentistry. Part 1: Focus on nanocomposite restoratives and biomimetics. Clinical, Cosmetic and Investigational Dentistry: November 2009 , Volume 2009:1 Pages 47 – 61.
3. Gordon, Mondragon, et. al. A Clinical evaluation of a self-etching primer and a giomer restorative material. Results at eight years. JADA(138) May 2007, p 621-627. 4. Gordan, V. et al, ed. IADR General Session. Seattle, Washington State Convention Center. March 23 2013. Clinical Evaluation of a Giomer Restorative System: Thirteen-Year Recall. Poster Session.
John C. Comisi, DDS, is a graduate of Northwestern University Dental School and has been in private practice of General Dentistry since 1983 in Ithaca, NY. He is a Master of the Academy of General Dentistry, and lectures on various dental topics and procedures. Reach him at email: [email protected].
Past DE Issues
About the Author
John Comisi, DDS, MAGD
John Comisi, DDS, MAGD, practiced dentistry in Ithaca, New York, for more than 30 years. Today he is an associate professor of restorative dentistry in the Department of Oral Rehabilitation at the Medical University of South Carolina. He speaks and writes on a variety of topics and is a consultant for companies in the dental industry.