By Charles Rodgers, DDS
We have surpassed the point in patient care where most clinicians choose composites over amalgams for their prospective patient care. This can easily be seen by insurance carrier utilization reports. And yet, I still occasionally hear dentists state an amalgam is "good enough." Though quite possibly a true statement, who among us would choose the most basic and cheapest tire for our cars? If costs were equal to patient and provider, which of us would choose the ceramic inlay over the amalgam?
We are now receiving notice that our go-to restoration choice -- composite -- is also losing its luster. Multiple research studies are confirming less than stellar outcomes when looking at broad averages. Agreed, without doubt an appropriately chosen size and properly placed composite can be a great choice, but large numbers of restorations placed by many providers are not supporting our expectations for this material. Is composite a superior choice to amalgam? When based on appearance alone, that is true without question. Now look at the ceramic inlay. Based on longevity, it becomes murkier. Again, what if costs were equal to patient and provider, which of us would choose the ceramic inlay over the composite? What if chairside efficiency for dentist and patient to place the inlay were comparable to the composite?
Should the patient's financial ability to pay affect our recommended treatments? Should the clinician's perception of the patient's wallet affect our recommended treatments? I would hope the answer to both questions would be a resounding "no," but along with the allowance for lesser treatment choices, there is no way to avoid it. What if we could charge the exact same amount for a composite and a CAD/CAM inlay? I submit that most dentists would choose the CAD/CAM. In fact, I get consistent feedback from practitioners that if the cost of inlays were comparable to the cost of composites, they would choose ceramic-based inlays most of the time. Of course, my feedback may be biased by the fact that all the dentists I communicate with have access to CAD/CAM. Ironically, when the price spread is large between the choices, it is typically followed by accusations of dentists trying to make more money, or gouge the patient. I say "ironic" because we are all patients at some point, and as a patient, I want to know what my best choices are, even if I ultimately choose a lesser alternative for my treatment.
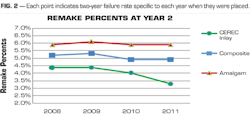
Many of you may have seen a recent industry journal article stating a two-year failure rate of amalgams and composites at 6.2%. This study involved more than 200 dentists. It continued by stating that there was not a significant difference between amalgams and composite failure rates at the two-year mark. I imagine many saw this particular percentage too high or even thought this is some other dentist, not me. I think the more crucial learning here is, "How can we, as clinical care providers, impact and lower the failure rate of restorations?" and "What materials will lead the future in this category of clinical procedural care?" While hearing of the survival or failure rates attributed to various restoration choices, it can cause us to self-reflect on our own preferred procedure choices and the resultant outcomes. This helps us reconsider not only which choices seemed to be the best at placement, but also which choices were tied to measurably better success rates over time.
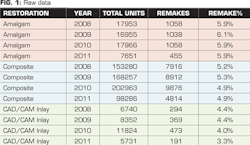
Pacific Dental Services® (PDS®)-supported dentists have been placing CEREC CAD/CAM-based restorations for seven years. There are a large number of restorations that can be evaluated. To get the best comparison across sequential years, we chose to look at the two-year remake rate for each year that they had been placed. Of course, to measure a two-year remake rate, the restorations need to be at least two years old. The data points we will be looking at are from the four-year period of 2008 to 2011. The remake percentage includes any remake done for whatever reason deemed necessary by the treating dentist. This includes remakes due to wear, cracking, fracture, loss, and even the occasional remake solely due to patient cosmetic concerns, as all are tracked with the same code in our software.
- The statistics for 2011 are roughly half of the prior years' due to the fact this is a two-year evaluation and at the time of this writing 2013 is only half over.
As can be seen by the graph in Figure 2, the remake rate of composite and amalgam restorations being placed by PDS-supported dentists over the course of four years has basically stayed level, while the two-year remake percentage tied to CAD/CAM inlays started at a lower point and is continuing downward.
Conjectured reasons regarding this ongoing decrease in remake rates for CAD/CAM inlays:
- The large increase in the number of inlays being provided has allowed repetition of procedure by each provider promoting more consistent delivery and outcomes.
- The use of digital technologies has allowed greatly magnified viewing of prep design encouraging self-evaluation and improvement of prep skills.
- The use of digital technologies provides the chance to dissect prep design as well as proposed restorations through means of depth and cross-sectional analysis.
- The use of digital technologies provides capability of more accurate fitting of final restorations.
- CAD/CAM choices of milling materials are expanding, exponentially allowing practitioners to more specifically cater materials to match patient needs.
Any recent convention attendee will confirm the plethora of imaging systems being offered. A dental lab convention attendee will see even more imaging choices offered to them. There is no doubt the industry is rapidly heading down the digital imaging path. With the increase in imaging choices, a decrease in related costs will follow along with more versatility for the provider to choose where to place their technologies in the patient flow process. It could be a connection to send an image to a lab or an excuse to buy an in-house mill and start making restorations on-site. With the increase in imaging choices, you will see improved ease of use as manufacturers pursue convenience for their future customers. With ease of use, you will see increased chairside efficiencies. Simultaneously, we have increasing choices of ceramic type materials with which to mill and restore. This will all come with a reduction in failures and remakes, equating to one more additional cost-savings category for the dentist, staff, and the whole treating facility. Patients will also see the benefits of not having to visit the dentist as much since the failure rates for remakes are down.
With all of these shifts happening, we can also expect the average cost of placing inlays and onlays to decrease. This will tie to a decrease to the average cost the consumer bears as well. With more leveling out of pricing, practitioners will be more willing to promote the ceramic choices over the composite-based ones.
To positively impact procedural results requires more consistent and predictable outcomes across large segments of patient care and procedure choices. It requires removing guesswork out of the hands of practitioners. It demands digital choices over analog whenever possible. Increasing ease of product use must also be a component of these procedures. All of these combined with reasonable and justifiable cost factors, the costs to initiate the technologies as well as the costs to integrate for maximum utilization.
All of us have selectively volunteered and been tasked with offering and placing the best restoration treatments for our patients. Sadly, too often, the patient is offered the "least cost" alternative with only a brief discussion of the "best choice" alternative. There is a multitude of reasons for this but it seems the clear focus comes when we place ourselves into the consumer role. I want to know what my best choices are, always, whether buying a car, television, or computer. I especially want to know my best choices when they involve the health of my family or myself.
While it depends on what study you evaluate, the failure rate for fillings in the dental industry seems to consistently hover around 5%. Does this seem reasonable? Is this part of the inherent risk with these type of procedures? Why 5% and not 10% or 3%? Yes, the higher-risk restorations result in an even higher failure rate. What is in our heads that allows us to believe that these types of failure rates are acceptable?
How do we compare with another industry, such as the airlines? The failure rate that is referenced in regard to air travel is commonly quoted as 1 in 10 million. The proverbial Six Sigma, and perhaps thankfully so. Some may consider this is not a fair comparison. What about something much simpler such as the airlines lost luggage rate? The lost luggage rate in the airline industry is roughly three bags out of 1,000, which translates into 0.3% -- a fraction of a single percent. This is less than one tenth of most referenced dental studies on procedure failures. This is dramatically better than our industry failure rates for each of fillings, crowns, and root canals. We are long overdue to have higher expectations and results for ourselves and our industry as a whole.
There is clear evidence among PDS-supported dentists of a lower initial remake rate with CAD/CAM inlays in comparison to traditional restoration materials, along with an ever decreasing remake rate among CAD/CAM inlays as measured at the two-year mark. The current trends also support a favorable downward trajectory of remakes. With increased choices of digital imaging technologies will come reduced related costs, increased efficiencies, and most notably a shift in preferred treatment recommendations by providers as they embrace ease of use with the best long-term patient care solutions.
Charles Rodgers, DDS, is vice president of clinicians for Pacific Dental Services (PDS). A 1987 graduate of Loma Linda University School of Dentistry, he has been supported by PDS since 1994. He is a member of the ADA, CDA, Orange County Dental Society, and American Academy of Oral Systemic Health. You may contact him by email at [email protected].
Past DE Articles