Building the foundation for your practice through grafting
by Ara Nazarian, DDS, DICOI
In my practice, which is located in the suburbs of Michigan, we have patients present with a tooth requiring an extraction at least three or four times a week. Whether it's due to severe decay or periodontal disease, the teeth are no longer considered restorable and require removal. With the increase in patients who present with these types of problems, it is essential for dentists to implement bone grafting as an adjunctive procedure to extractions in order to set the foundation for future dental implant and reconstructive treatment. Not only are you providing a great service for your patients, you're also increasing your practice's economic potential.
Bone grafting is the replacement or augmentation of the portion of the jawbone that anchors the teeth. This surgical procedure is done to reverse the loss or resorption of bone, which may have occurred due to tooth loss, trauma, or disease, and to rebuild the bone structure beneath the gums to prepare for the placement of dental implants or other tooth replacements.
When bone graft is placed in the jaw, it doesn't just simply fill a void in the bone; it may also help promote new bone growth in that location. When successful, bone grafting restores both the height and width of a patient's jawbone.
With over 20 million teeth needing extractions each year in North America, more general dentists can increase their practice potential and serve their patients by performing the extraction and grafting themselves, if they receive the proper training.
In the example in the photos, a patient presented with severely broken down and decayed teeth in Nos. 3 and 5 (Fig. 1). She mentioned that the previous bridge from Nos. 3 through 5 broke off three months earlier. But since the teeth had previous endodontic therapy, she had no pain. All risks, benefits, and alternatives were reviewed with the patient. Due to the gross decay and little remaining tooth structure, we advised that the teeth be extracted and the area grafted for future implant placement with corresponding abutments and crowns. Not only did the patient accept this treatment, she was pleased that it would all be done at one location.
Our goal in removing these teeth was to preserve as much surrounding bone as possible during the extractions, followed by grafting the area to increase height and width of the alveolar ridge. The key to successful site preservation is minimizing any trauma to the hard and soft tissues around the teeth being extracted. In order to achieve this, it was necessary to adopt the appropriate technique and instrumentation.
Acting simply like a class I lever, only one force must be applied to the beak of the Physics Forceps (Golden Dental Solutions). The beak grasped the tooth, while the bumper acted as the fulcrum to provide leverage and stability for the beak. Once the (UR) Physics Forceps instrument was properly placed, pressure was slowly applied using only wrist movement. During this holding period, the internal force increased and allowed the bone to slowly expand and the periodontal ligament to release, at which point the tooth disengaged from its socket (Fig. 2).
Once the teeth were extracted, it was imperative to thoroughly debride the socket walls, so the areas were cleaned of any granulation tissue with a curette (Zoll-Dental) and irrigated with sterile saline. This part of the procedure should not be rushed; each area within the extraction socket needs to be curetted and all remnant periodontal ligament tissues removed from the socket walls. This also has the added advantage of inducing some bleeding (increased vascularity) into the socket.
Using a bone bur (ACE Surgical), the residual ridge in the area of the pontic site was decorticated, which I routinely do as part of a guided bone regeneration (GBR) procedure in a deficient site. The biologic rationale for decortication of bone is to allow progenitor cells easy access to a GBR-treated site and to facilitate prompt angiogenesis. It also enhances the physical connection between a bone graft and a recipient site.
A number of different materials have been suggested for use in extraction sockets; however, not all are suitable.1 What is used should be based on biological principles. A graft material should be biocompatible, support bone growth, and be resorbable. The material used for socket augmentation should support vital bone formation into the socket in order to allow for successful osseointegration of the dental implant that will be placed into the site. Thus, it is preferable that the material is resorbable and ultimately replaced with vital bone long-term.2
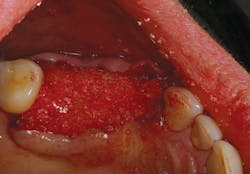
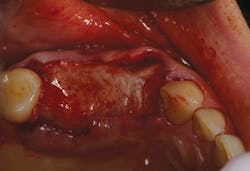
Bone grafting material (NuOss, ACE Surgical) was placed into the clean socket and pontic area (Fig. 3). To assist with containment of the graft particles within the surgical site, a resorbable barrier membrane (ConFORM, ACE Surgical) was used (Fig. 4). The principle purpose of the barrier membrane is to contain the graft material, while soft-tissue healing takes place over the surgical site. The edge of the membrane was tucked under the flap on the buccal/labial and palatal aspects. Interrupted sutures were then used to adapt the marginal soft tissues over the barrier membrane (Fig. 5).
It is important to note that implant placement into a previously grafted extraction site should not be sooner than four months postextraction to allow for sufficient healing and consolidation of the bone through the grafted socket, and to ensure good initial stability of the implant at placement.
Today we have the ability to grow bone where needed. This not only gives us the opportunity to place implants of proper length and width; it also gives us a chance to restore functionality and esthetic appearance for our patients. If you don't currently offer extractions and grafting, I highly recommend getting the training in order to implement these services into your practice.
References
1. Froum S, Orlowski W. Ridge preservation utilizing an alloplast prior to implant placement - clinical and histological case reports. Pract Periodontics Aesthet Dent. 2000 May;12(4):393-402; quiz 404.
2. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003; 74(7):990-999.
Ara Nazarian, DDS, maintains a private practice in Troy, Mich., with an emphasis on comprehensive and restorative care. He has earned a Fellowship and Mastership in the International Congress of Oral Implantologists (ICOI). His articles have been published in many of today's popular dental publications. Dr. Nazarian is the director of the Reconstructive Dentistry Institute. He has conducted lectures and hands-on workshops on esthetic materials and dental implants throughout the U.S., Europe, New Zealand, and Australia. Dr. Nazarian is also the creator of the DemoDent patient education model system. He can be reached at (248) 457-0500 or at the website www.aranazariandds.com.